Share Year Notice For Free
Drop document here to upload
Up to 100 MB for PDF and up to 25 MB for DOC, DOCX, RTF, PPT, PPTX, JPEG, PNG, JFIF, XLS, XLSX or TXT
Note: Integration described on this webpage may temporarily not be available.
0
Forms filled
0
Forms signed
0
Forms sent
Discover the simplicity of processing PDFs online
Upload your document in seconds
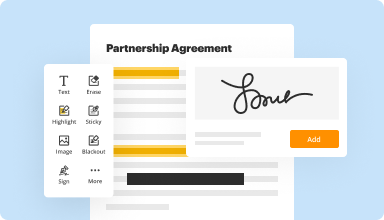
Fill out, edit, or eSign your PDF hassle-free

Download, export, or share your edited file instantly
Top-rated PDF software recognized for its ease of use, powerful features, and impeccable support






Every PDF tool you need to get documents done paper-free
Create & edit PDFs
Generate new PDFs from scratch or transform existing documents into reusable templates. Type anywhere on a PDF, rewrite original PDF content, insert images or graphics, redact sensitive details, and highlight important information using an intuitive online editor.
Fill out & sign PDF forms
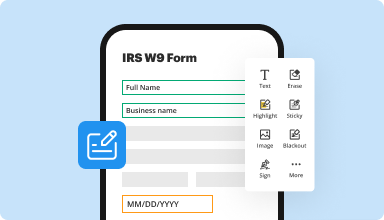
Say goodbye to error-prone manual hassles. Complete any PDF document electronically – even while on the go. Pre-fill multiple PDFs simultaneously or extract responses from completed forms with ease.
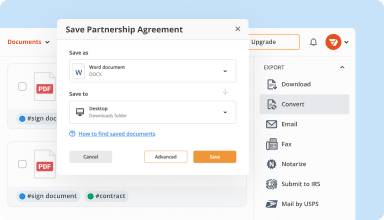
Organize & convert PDFs
Add, remove, or rearrange pages inside your PDFs in seconds. Create new documents by merging or splitting PDFs. Instantly convert edited files to various formats when you download or export them.
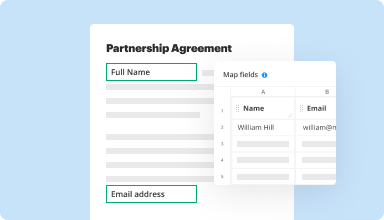
Collect data and approvals
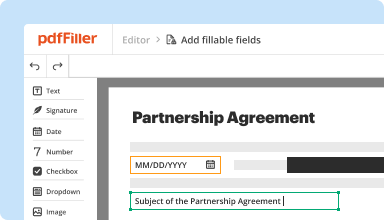
Transform static documents into interactive fillable forms by dragging and dropping various types of fillable fields on your PDFs. Publish these forms on websites or share them via a direct link to capture data, collect signatures, and request payments.
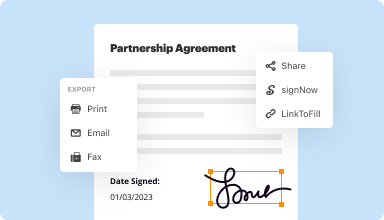
Export documents with ease
Share, email, print, fax, or download edited documents in just a few clicks. Quickly export and import documents from popular cloud storage services like Google Drive, Box, and Dropbox.
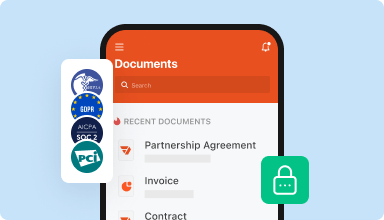
Store documents safely
Store an unlimited number of documents and templates securely in the cloud and access them from any location or device. Add an extra level of protection to documents by locking them with a password, placing them in encrypted folders, or requesting user authentication.
Customer trust by the numbers
64M+
users worldwide
4.6/5
average user rating
4M
PDFs edited per month
9 min
average to create and edit a PDF
Join 64+ million people using paperless workflows to drive productivity and cut costs
Why choose our PDF solution?
Cloud-native PDF editor
Access powerful PDF tools, as well as your documents and templates, from anywhere. No installation needed.
Top-rated for ease of use
Create, edit, and fill out PDF documents faster with an intuitive UI that only takes minutes to master.
Industry-leading customer service
Enjoy peace of mind with an award-winning customer support team always within reach.
What our customers say about pdfFiller
See for yourself by reading reviews on the most popular resources:
I needed to update a PDF document to look neat and clean and PDF filler was quick and easy to use and easy to get to because it is web base. I love it
2017-07-16
Great program for your doc management, font adjustments,varies tools availability can address an assortment of issues to make your paperwork look professional every time,and it is very user friendly. Thanks
2017-10-05
This app is great. I can handle all of my business's contract signing operations and form generation with one tool! I would like to see more mobile app functionality.
2019-01-17
great customer service - sam
great, easy to use, saves us a fortune on an extra phone line for a fax. Great customer service, I always use live chat and get answers and resolution within a few minutes. I have only had to use support 3 times in a year because the program is so user friendly.
2019-03-29
Great product to add a professional look to your completed documents
Adds a quality appearance to my work.
No more manual handwriting ugly forms. Once the user is able to follow the print/save process the end product is quickly achieved.
Quality finished product when using PDF-Filler. The software easily converts rough looking hard to read forms into easy to follow wordsmith quality documents.
2017-11-14
easy to use
easy to use, it would be good if you could copy text and paste it i might not have worked out how to do that yet if its there, and insert signature would be helpful, that might be there already but i couldnt find it otherwise its easy to use and easy to send documents
2022-02-16
I love it
I love it! I've been using PDFiller for my business for over two years. You will be surprised all the advantages it has to offer for documents. Enjoy!
2022-02-08
Basically does what I need
Basically does what I need. Could use better Help function. Example: I haven't figured out how to control the type font used nor how to match existing fonts in a document.
2021-12-29
What do you like best?
I like being able to alter PDFs and forms
What do you dislike?
yearly subscription is expensive and costly
What problems are you solving with the product? What benefits have you realized?
It makes it much easier for me to complete forms.
2020-08-30
Share Year Notice Feature
The Share Year Notice feature simplifies how you communicate important information to your team or clients. This tool allows you to share annual updates smoothly, ensuring everyone stays informed.
Key Features
Easy sharing of annual reports and updates
Customizable templates for clear communication
Automatic reminders for key deadlines
Track engagement to see who has accessed materials
User-friendly interface for quick setup
Potential Use Cases and Benefits
Ideal for organizations sharing yearly performance summaries
Helpful for teams needing to review project outcomes
Useful for clients wanting updates on service milestones
Great for maintaining transparency and engagement
Supports strategic planning by keeping stakeholders informed
With the Share Year Notice feature, you solve the challenge of keeping everyone aligned and engaged. You no longer have to worry about missed communications or confusion. Instead, effortlessly manage information sharing to enhance understanding and cooperation within your team and with your clients.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What if I have more questions?
Contact Support
Who should receive an initial Cobra notice?
A group health plan subject to COBRA is required to provide an initial (or general) COBRA notice to a covered employee or covered spouse only once within 90 days after the individual first becomes covered under the plan. (There is no requirement to provide an initial notice to dependent children.)
Do initial Cobra notices need to be mailed?
COBRA ADMINISTRATION REQUIRES PROPER DELIVERY OF NOTICES. The initial (or general) notice containing information about COBRA rights and responsibilities, which must be provided to the employee and spouse within 90 days of when the employee first becomes covered under the plan.
When must Cobra notices be sent out?
Plan administrators must provide a written general notice of COBRA rights to each covered employee and spouse (if any) within 90 days after their coverage under a GAP begins. The general notice must also be sent to any new dependents added to the plan after the employee's initial enrollment.
What is a Cobra initial notice?
Did you know that one of the most important COBRA notices is the initial notice, or what is referred to as the general rights notice? The initial notice communicates to plan participants their COBRA rights and obligations and must be furnished by the plan administrator within 90 days after coverage begins.
What does it mean when you get a cobra letter in the mail?
Why did I receive A COBRA Letter? A: There are a few reasons you've received a Cobra Notification. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
Who provides you with the initial general notice about Cobra benefits?
This notice is issued by the plan administrator within the first 90 days when coverage begins under the group health plan and informs the covered employee (and his or her spouse) of the responsibility to notify the employer within 60 days if certain qualifying events occur in the future.
Why would I receive a cobra letter?
Q: Why did I receive A COBRA Letter? The purpose of this letter is to inform you of your rights and responsibilities as a plan participant. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
What is a Cobra rights notice?
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Video Review on How to Share Year Notice
#1 usability according to G2
Try the PDF solution that respects your time.






