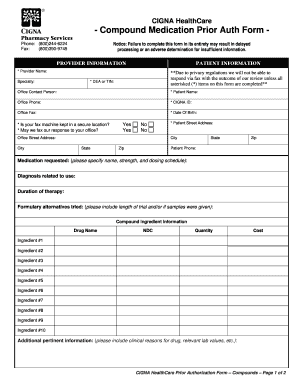
Cigna Authorization Forms
What is cigna authorization forms?
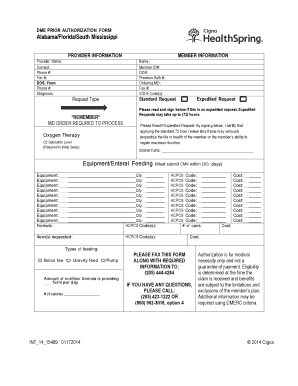
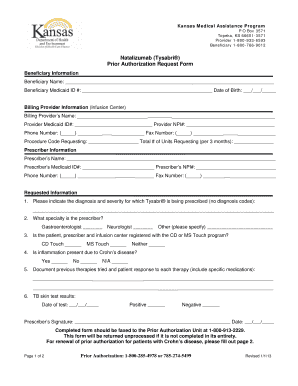
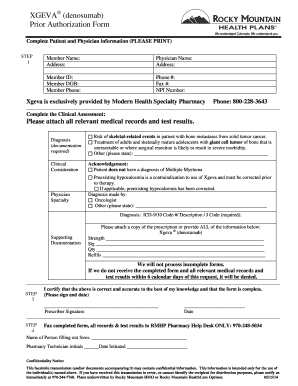
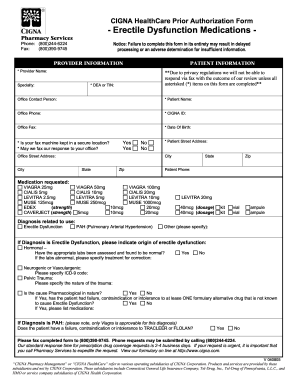
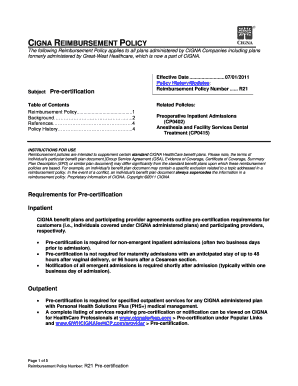
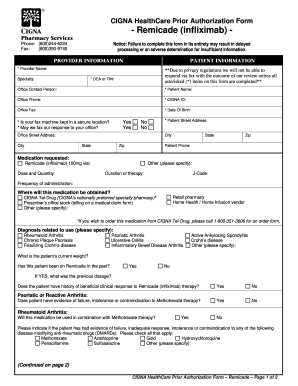
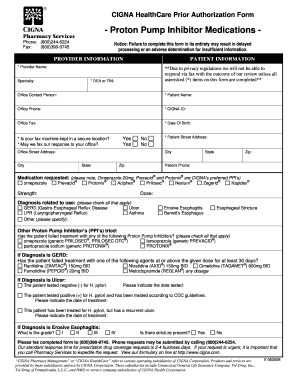
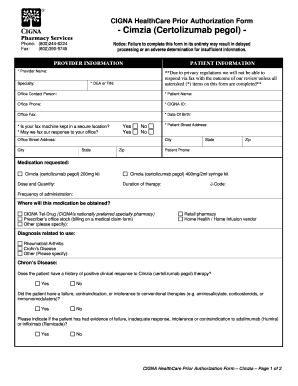
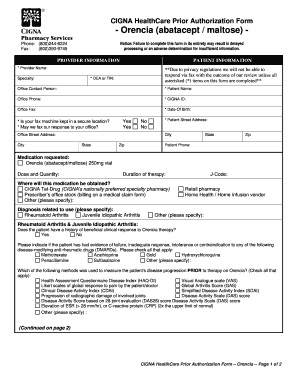
Cigna authorization forms are important documents that provide consent for medical procedures, treatments, or services. These forms are typically required by healthcare providers or insurance companies to ensure that the necessary procedures are authorized and covered by the insurance policy. By signing a Cigna authorization form, patients give their permission for the healthcare provider to access and disclose their medical information as required for the specified treatment or service.
What are the types of cigna authorization forms?
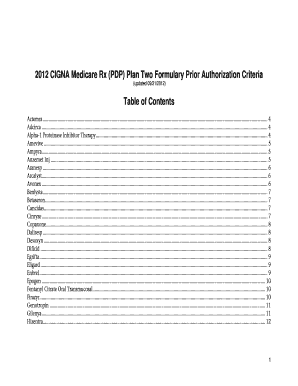
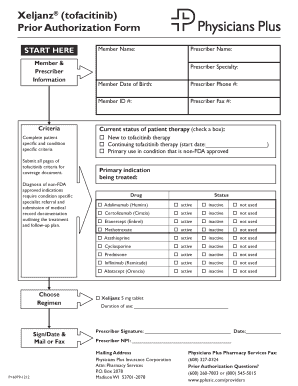
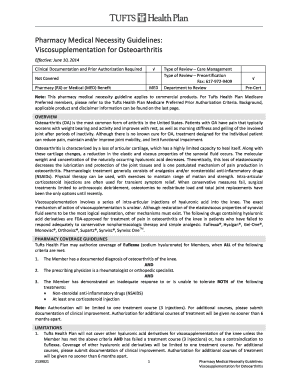
Cigna offers various types of authorization forms that cater to different healthcare needs. Some common types of Cigna authorization forms include:
How to complete cigna authorization forms
Completing Cigna authorization forms is a straightforward process. Here's a step-by-step guide to help you:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.