Get the free 277 Claim Acknowledgment
Show details
This implementation guide provides data requirements and content for receivers of Highmark's version of the 277 - Claim Acknowledgment Transaction, focusing on use as an acknowledgment of claim submission(s).
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign 277 claim acknowledgment
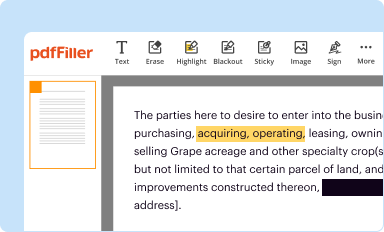
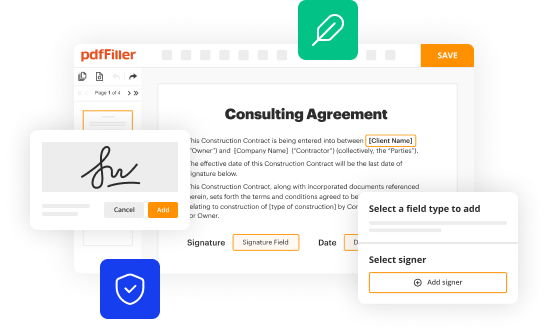
Edit your 277 claim acknowledgment form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
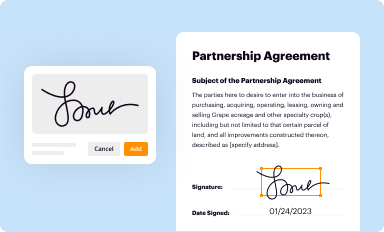
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
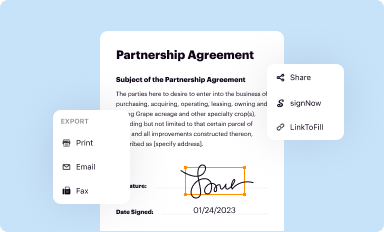
Share your form instantly
Email, fax, or share your 277 claim acknowledgment form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing 277 claim acknowledgment online
Follow the guidelines below to benefit from a competent PDF editor:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit 277 claim acknowledgment. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
Dealing with documents is always simple with pdfFiller.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out 277 claim acknowledgment
How to fill out 277 Claim Acknowledgment
01
Start by gathering the required patient and claim information.
02
Fill out the patient's identification details including name, date of birth, and insurance ID.
03
Enter the claim information such as claim number, date of service, and procedure codes.
04
Provide the payer's information including name and any necessary identification numbers.
05
Indicate the status of the claim (e.g., received, under review, denied, etc.).
06
Review all information for accuracy and completeness before submission.
07
Submit the 277 Claim Acknowledgment to the appropriate payer.
Who needs 277 Claim Acknowledgment?
01
Healthcare providers submitting claims to insurance payers.
02
Insurance companies processing the claims for payment.
03
Billing and coding professionals managing medical claims.
Fill
form
: Try Risk Free






People Also Ask about
What is a 277 in healthcare?
The EDI 277 transaction is an electronic Healthcare Claim Status Notification (also known as ANSI X12 EDI 277). An EDI 277 Healthcare Claim Status Notification is sent by the healthcare insurance company/payor to report on the status of claims that were previously submitted by healthcare providers.
What is claim Acknowledgement?
The 277 response provides updates on the claim's status, indicating whether it is: Accepted: Under review by the payer. Denied: The claim was rejected with an explanation. Pending: Additional information is required.
What is the denial code 277?
Denial code 277 is used when the disposition of a claim or service is undetermined during the premium payment grace period, as required by the Health Insurance SHOP Exchange.
What is the difference between 999 and 277?
Whereas the 999 - Acknowledgement confirms receipt of a transaction (in this case the 837), the 277CA provides more specific information about the claims that were contained in the 837, e.g. the unique identifier assigned by the health plan to their claims (i.e. per the TR3 - the payor claim control number).
What is the Medicare denial code 277?
Denial code 277 is used when the disposition of a claim or service is undetermined during the premium payment grace period, as required by the Health Insurance SHOP Exchange.
What is a 277 claim status response?
The 277 Response uses the Claim Status Category Codes and Status Codes to identify security validation requirement issues and to indicate BCBSNC business edits. The following table lists all codes supported by BCBSNC within the 277 Transaction, Loop 2200D or 2200E, Elements STC01-1 and STC01-2.
What is a 277 payer response?
The EDI 277 transaction is an electronic Healthcare Claim Status Notification (also known as ANSI X12 EDI 277). An EDI 277 Healthcare Claim Status Notification is sent by the healthcare insurance company/payor to report on the status of claims that were previously submitted by healthcare providers.
What is the EDI 277 claim status?
The EDI 277 transaction is an electronic Healthcare Claim Status Notification (also known as ANSI X12 EDI 277). An EDI 277 Healthcare Claim Status Notification is sent by the healthcare insurance company/payor to report on the status of claims that were previously submitted by healthcare providers.
What is the reason for denial code 227?
Denial code 227 means that the requested information from the patient, insured, or responsible party was either not provided or was insufficient or incomplete. In order to process the claim, at least one Remark Code must be provided.
What is the 277 transaction code set?
The EDI 277 transaction set can either be used as an insurance company's electronic response to a previously received EDI 276-A1 or to request additional information from a healthcare provider without a submitted claim. It is generally used by healthcare payers such as insurance companies, Medicare, and others.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is 277 Claim Acknowledgment?
277 Claim Acknowledgment is a standard transaction set used in the healthcare industry to report the status of medical claims. It provides feedback to healthcare providers regarding the claims they have submitted.
Who is required to file 277 Claim Acknowledgment?
Payers, such as insurance companies or government programs, are required to file 277 Claim Acknowledgment. They send this acknowledgment to healthcare providers to confirm receipt and status of submitted claims.
How to fill out 277 Claim Acknowledgment?
Filling out a 277 Claim Acknowledgment involves inputting specific claim status information, including claim identifiers, payer identification, and reasons for acceptance or rejection. It is formatted according to the standard requirements of the ASC X12 277 transaction.
What is the purpose of 277 Claim Acknowledgment?
The purpose of the 277 Claim Acknowledgment is to inform healthcare providers about the status of their claims, helping them to understand whether claims have been accepted, rejected, or require further action.
What information must be reported on 277 Claim Acknowledgment?
Information that must be reported includes claim status codes, claim identifiers, payer identifiers, and specific details regarding any issues or actions required on denied claims.
Fill out your 277 claim acknowledgment online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

277 Claim Acknowledgment is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.