Get the free progress notes soap form - med fsu
Show details
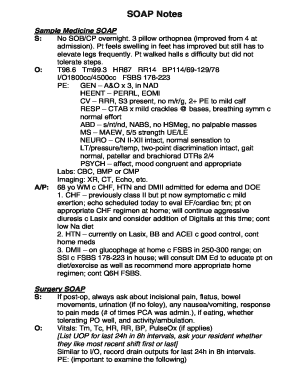
SOAP Notes Format in EMR SOAP stands for Subjective, Objective, Assessment, and Plan Standard Elements of SOAP note Date: 08/01/02 Time: Provider: Vital Signs: Height, Weight, Temp, B/P, Pulse S:
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign progress notes soap form
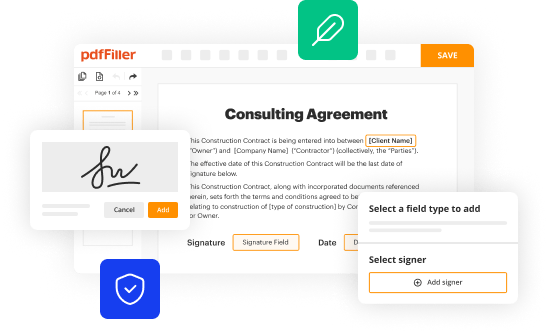
Edit your progress notes soap form form online
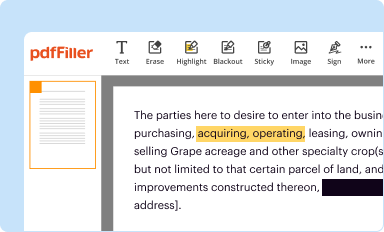
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
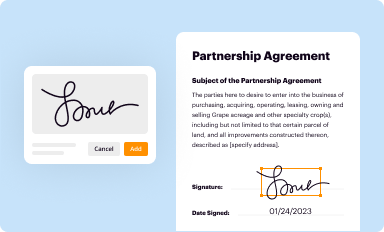
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
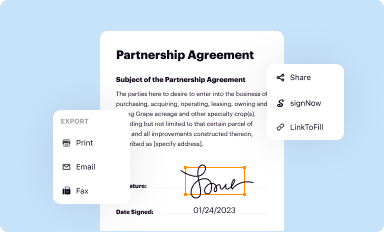
Share your form instantly
Email, fax, or share your progress notes soap form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit progress notes soap form online
To use our professional PDF editor, follow these steps:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit progress notes soap form. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out progress notes soap form
How to fill out a progress notes SOAP form:
01
Start by writing the date and time of the progress note at the top of the form.
02
Next, input the patient's name, date of birth, and any other relevant identification information.
03
Begin with the "Subjective" section, where you document the patient's complaints, symptoms, and concerns. This includes their own description of how they are feeling.
04
Move on to the "Objective" section, where you record any measurable and observable information such as vital signs, physical examination findings, and laboratory test results.
05
In the "Assessment" section, provide your professional evaluation and diagnosis based on the subjective and objective information gathered. This may include potential differential diagnoses.
06
Create a plan in the "Plan" section to address the patient's concerns and symptoms. This may include medications prescribed, referrals to specialists, or additional laboratory tests.
07
Finally, sign and date the progress note to authenticate its completion.
Who needs a progress notes SOAP form?
01
Healthcare professionals: doctors, nurses, therapists, and other healthcare providers need progress notes SOAP forms to accurately document their patients' medical history, assessment, and treatment plans.
02
Medical institutions: hospitals, clinics, and healthcare facilities require progress notes SOAP forms for record-keeping, continuity of care, and legal documentation purposes.
03
Medical billing and coding professionals: progress notes SOAP forms are essential for accurate coding and billing processes for patient visits and treatments. It helps ensure proper reimbursement and claims processing.
04
Insurance companies: progress notes SOAP forms can be used by insurance companies to verify the medical necessity of treatments and assess claim requests.
05
Academic institutions: medical schools and healthcare training programs use progress notes SOAP forms to teach students about patient assessment, diagnosis, and treatment planning.
In summary, filling out a progress notes SOAP form requires capturing subjective and objective information, assessing the patient's condition, creating a treatment plan, and authenticating the note. It is necessary for healthcare professionals, medical institutions, medical billing and coding professionals, insurance companies, and academic institutions.
Fill
form
: Try Risk Free
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an electronic signature for the progress notes soap form in Chrome?
Yes, you can. With pdfFiller, you not only get a feature-rich PDF editor and fillable form builder but a powerful e-signature solution that you can add directly to your Chrome browser. Using our extension, you can create your legally-binding eSignature by typing, drawing, or capturing a photo of your signature using your webcam. Choose whichever method you prefer and eSign your progress notes soap form in minutes.
Can I create an electronic signature for signing my progress notes soap form in Gmail?
Upload, type, or draw a signature in Gmail with the help of pdfFiller’s add-on. pdfFiller enables you to eSign your progress notes soap form and other documents right in your inbox. Register your account in order to save signed documents and your personal signatures.
How do I complete progress notes soap form on an iOS device?
Install the pdfFiller app on your iOS device to fill out papers. Create an account or log in if you already have one. After registering, upload your progress notes soap form. You may now use pdfFiller's advanced features like adding fillable fields and eSigning documents from any device, anywhere.
What is progress notes soap form?
Progress notes soap form is a documentation template used in healthcare settings to track a patient's progress, treatment, and outcomes.
Who is required to file progress notes soap form?
Healthcare professionals, such as doctors, nurses, and therapists, are required to file progress notes soap form for each patient they are treating.
How to fill out progress notes soap form?
To fill out progress notes soap form, one must document subjective information, objective observations, assessment of the patient's condition, and the plan for further treatment.
What is the purpose of progress notes soap form?
The purpose of progress notes soap form is to provide a comprehensive record of a patient's treatment, progress, and response to interventions.
What information must be reported on progress notes soap form?
Information such as patient's complaints, vital signs, diagnostic test results, clinical impressions, and treatment goals must be reported on progress notes soap form.
Fill out your progress notes soap form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Progress Notes Soap Form is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.