Get the free soap narrative ems
Show details
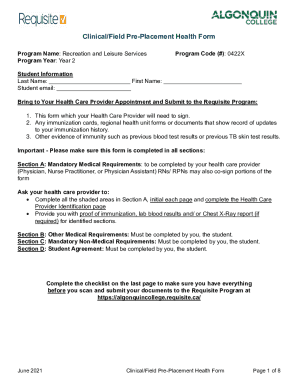
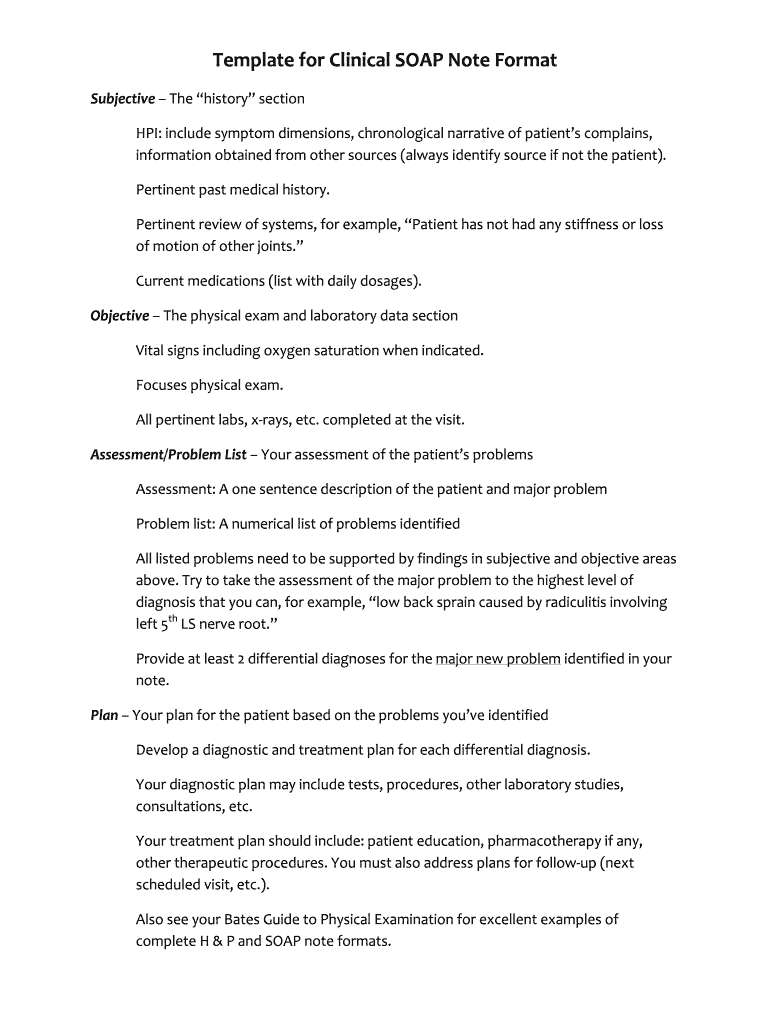
Template for Clinical SOAP Note Format Subjective The history section HPI include symptom dimensions chronological narrative of patient s complains information obtained from other sources always identify source if not the patient. Pertinent past medical history. Pertinent review of systems for example Patient has not had any stiffness or loss of motion of other joints. Current medications list with daily dosages. Objective The physical exam and laboratory data section Vital signs including...
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign soap narrative form
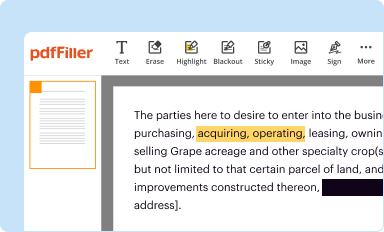
Edit your ems narrative examples soap form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
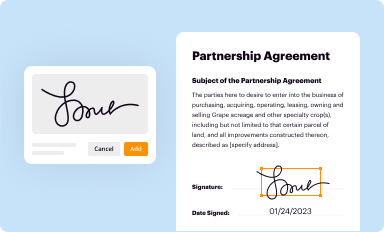
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
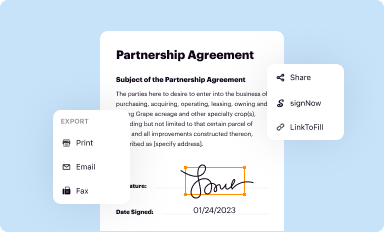
Share your form instantly
Email, fax, or share your soap narrative ems example form via URL. You can also download, print, or export forms to your preferred cloud storage service.
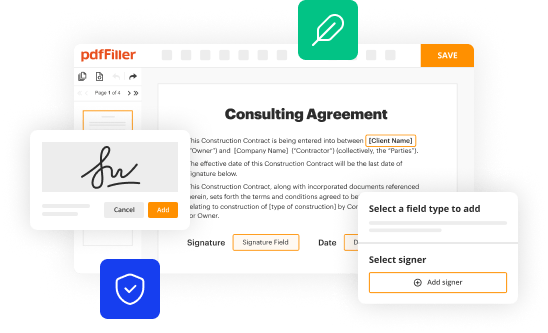
How to edit ems soap narrative examples online
To use the professional PDF editor, follow these steps:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit soap ems report example form. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
The use of pdfFiller makes dealing with documents straightforward.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out ems soap narrative form
To fill out a SOAP narrative, follow these steps:
01
Begin with the "Subjective" section: Write a detailed description of the patient's subjective complaints, symptoms, and any relevant history. Include information about the patient's current condition, previous treatments, and any concerns they may have.
02
Move on to the "Objective" section: Document the objective findings based on the patient's physical examination and any diagnostic tests or lab results. Include vital signs, physical observations, and any measurable data related to the patient's health.
03
Proceed to the "Assessment" section: Provide a summary of the healthcare professional's assessment of the patient's condition. This should include a diagnosis, if applicable, as well as any differential diagnoses considered.
04
Finally, write the "Plan" section: Outline the plan of action for the patient's treatment and management. This may include medication prescriptions, referrals to specialists, diagnostic tests, patient education, and any other interventions recommended.
Who needs soap narrative:
A SOAP narrative is used by healthcare professionals, including doctors, nurses, physical therapists, and other providers, to effectively document patient encounters and track their progress. It is typically used in medical settings, such as hospitals, clinics, and private practices, to maintain accurate and organized patient records. The SOAP narrative is essential for communication between healthcare providers, as well as for legal and billing purposes.
Fill
soap pcr example
: Try Risk Free






People Also Ask about narrative soap note example
How do you write a simple SOAP note?
SOAP Notes: A Step-By-Step Guide Chief or Primary Complaint, e.g. their condition, symptoms, or historical diagnoses. History of Present Illness, often further structured into onset, location, duration, characterization, alleviating and aggravating factors, radiation, temporal factors, and severity (OLDCARTS)
What is a narrative SOAP note?
What is a SOAP Note? A SOAP note is a written document that a healthcare professional creates to describe a session with a patient/client. The information included is: Subjective, Objective, Assessment, Plan (SOAP). Many fields rely on SOAP notes to transfer information between professionals.
What is SOAP style format?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan.
How do you write a SOAP narrative?
Tips for Effective SOAP Notes Find the appropriate time to write SOAP notes. Maintain a professional voice. Avoid overly wordy phrasing. Avoid biased overly positive or negative phrasing. Be specific and concise. Avoid overly subjective statement without evidence. Avoid pronoun confusion. Be accurate but nonjudgmental.
What are the 4 parts of SOAP?
SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.Plan Create a list of all of the patient's medical problems. Propose a plan to manage each problem you've identified.
How do you write in SOAP format?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
What are the different types of SOAP notes?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan.This includes: Vital signs. Physical exam findings. Laboratory data. Imaging results. Other diagnostic data. Recognition and review of the documentation of other clinicians.
Is a SOAP note a narrative note?
Nurses use several methods to create nurses' notes. One of the most popular formats nurses use in narrative charting is known as SOAPI, which stands for Subjective, Objective, Assessment, Plan, and Interventions.
What does the acronym SOAP stand for?
SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit soap pcr template from Google Drive?
Using pdfFiller with Google Docs allows you to create, amend, and sign documents straight from your Google Drive. The add-on turns your soap narrative example ems into a dynamic fillable form that you can manage and eSign from anywhere.
How do I make changes in soap report ems example?
pdfFiller not only lets you change the content of your files, but you can also change the number and order of pages. Upload your ems soap report example to the editor and make any changes in a few clicks. The editor lets you black out, type, and erase text in PDFs. You can also add images, sticky notes, and text boxes, as well as many other things.
How do I complete ems narrative template on an iOS device?
In order to fill out documents on your iOS device, install the pdfFiller app. Create an account or log in to an existing one if you have a subscription to the service. Once the registration process is complete, upload your ems soap report template. You now can take advantage of pdfFiller's advanced functionalities: adding fillable fields and eSigning documents, and accessing them from any device, wherever you are.
What is soap narrative?
SOAP narrative is a structured method used in healthcare documentation to organize patient information into four categories: Subjective, Objective, Assessment, and Plan. This format helps healthcare providers communicate effectively and ensures that all relevant details are noted.
Who is required to file soap narrative?
Healthcare professionals involved in patient care, such as doctors, nurses, and therapists, are required to file SOAP narratives as part of their medical documentation to ensure continuity of care and accurate medical records.
How to fill out soap narrative?
To fill out a SOAP narrative, first document the Subjective information from the patient, including their symptoms and concerns. Next, record Objective findings from physical examinations and diagnostic tests. Then, provide an Assessment summarizing the clinical interpretation of the information collected. Finally, outline the Plan for treatment or further assessments.
What is the purpose of soap narrative?
The purpose of a SOAP narrative is to provide a clear, organized approach to documenting patient interactions and clinical observations, which facilitates communication among healthcare providers and helps in tracking patient progress.
What information must be reported on soap narrative?
The information reported in a SOAP narrative includes the patient’s subjective statements and complaints, objective findings from clinical examinations and tests, the clinician's assessment of the patient's condition, and the plan for future treatment or management of the patient's health.
Fill out your soap narrative ems form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Pcr Narrative Example is not the form you're looking for?Search for another form here.
Keywords relevant to pcr narrative template
Related to soap narrative template
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.