
Get the free MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM - floridalegal
Show details
This form is used for clients to provide information regarding the denial of their Medicaid prescription drug coverage, facilitating the process of addressing and resolving their issues through a
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign medicaid prescription drug denial
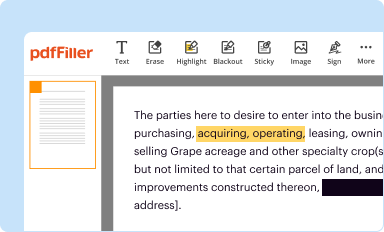
Edit your medicaid prescription drug denial form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
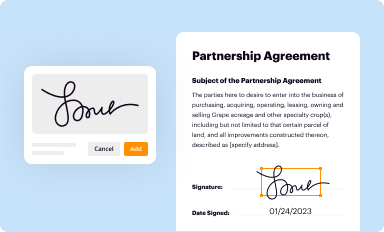
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
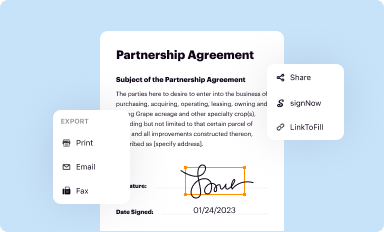
Share your form instantly
Email, fax, or share your medicaid prescription drug denial form via URL. You can also download, print, or export forms to your preferred cloud storage service.
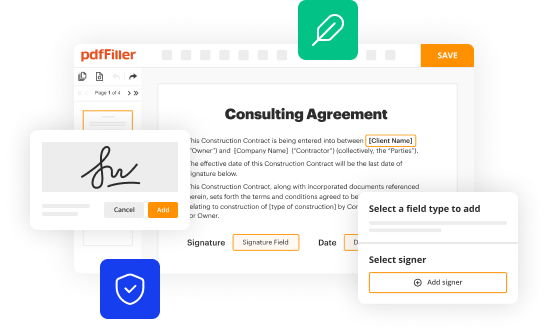
Editing medicaid prescription drug denial online
Follow the steps down below to benefit from the PDF editor's expertise:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit medicaid prescription drug denial. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
With pdfFiller, dealing with documents is always straightforward. Try it now!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out medicaid prescription drug denial
How to fill out MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM
01
Gather relevant personal information about the client, including name, address, and Medicaid ID.
02
Fill out the date of the request and provide contact information for the healthcare provider.
03
Indicate the specific prescription drug that has been denied and the reason for the denial.
04
Provide any relevant medical history or documentation that supports the need for the medication.
05
Include details of any previous attempts to obtain the medication or related issues.
06
Review the completed form for accuracy and completeness.
07
Submit the form to the appropriate Medicaid office or authority.
Who needs MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM?
01
Individuals who have had their prescribed medications denied by Medicaid.
02
Healthcare providers who need to appeal a Medicaid denial for a client's prescription.
03
Caregivers or family members assisting clients with medication management and appeals.
Fill
form
: Try Risk Free






People Also Ask about
Why would Medicaid deny a prescription?
Medicaid patients are increasingly facing procedural prescription denials, meaning their health plans refuse to cover medications for administrative reasons like early refills, plan limits on pill amounts or prior authorization rules.
What is the declaration of prescription drug coverage form?
The Declaration of Prior Prescription Drug Coverage is an essential form that Medicare requires to verify that you have had continuous prescription drug coverage. If you have received a letter requesting you to complete the form, make sure to provide the dates and name of the health insurance plan you had.
What is a proof of creditable coverage document?
A written certificate issued by a group health plan or health insurance issuer (including an HMO) that shows your prior health coverage (creditable coverage).
What to do if Medicaid doesn't cover medication?
Call the Medicaid Prescription Drug Helpline at 1-800-436-6001 for assistance if Medicaid or your Medicaid HMO will not cover your prescription. Call as soon as possible to prevent a disruption of your prescription drug coverage.
Why did Medicare deny my prescription?
If your plan made an error, they should correct it. If not, there are a few common reasons a plan may deny payment: Prior authorization: you must get prior approval from the plan before it will cover a specific drug. Step therapy: your plan requires you try a different or less expensive drug first.
What is the declaration of prescription drug coverage?
The Declaration of Prior Prescription Drug Coverage is an essential form that Medicare requires to verify that you have had continuous prescription drug coverage. If you have received a letter requesting you to complete the form, make sure to provide the dates and name of the health insurance plan you had.
Is Medicare Part D really necessary?
No, Medicare Part D isn't a requirement. However, many people find that enrolling in a Part D plan is worth the investment. Your health can be unpredictable, so while you may not need many (or any) prescription drugs now, you may need them in the future.
Why would a prescription be denied?
In general, a pharmacist can refuse to fill a prescription for the following reasons: The prescription isn't considered standard care or therapy. The prescription is likely to cause harm because its risks clearly outweigh the benefits. The pharmacist is having trouble verifying the prescription's validity.
What is a prescription drug claim form?
Prescription Drug Claim Form. Please use this form when you paid for a Medicare Part D covered prescription drug and are asking us to pay you back. Check your Evidence of Coverage (EOC) for more details on completing this form.
Why is Medicaid denying my prescription?
Errors in the prescription itself, missing information, or discrepancies between the prescribed medication and what Medicaid covers can all lead to a denial.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM?
The MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM is a document used to assess and collect information regarding clients who have been denied coverage for prescription medication under Medicaid.
Who is required to file MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM?
Healthcare providers, pharmacists, or authorized representatives of Medicaid clients who experience a denial for prescription drugs are required to file this form.
How to fill out MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM?
To fill out the form, gather relevant client information, including demographics, details of the denied prescription drug, the reason for denial, and any supporting documentation. Ensure that all required fields are accurately completed before submission.
What is the purpose of MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM?
The purpose of the form is to facilitate the review of Medicaid prescription drug denials, allowing for the documentation of client details and the specific circumstances surrounding the denial, which helps in processing appeals or requests for reconsideration.
What information must be reported on MEDICAID PRESCRIPTION DRUG DENIAL: CLIENT INTAKE SCREENING FORM?
Information required includes the client's name, Medicaid ID number, drug information, details of the denial (including dates and reasons), and any relevant healthcare provider or pharmacy information.
Fill out your medicaid prescription drug denial online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Medicaid Prescription Drug Denial is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















