Get the free Provider Enrollment FAQs
Show details
This document provides answers to frequently asked questions regarding provider enrollment for Medicaid, detailing requirements, procedures, and guidelines for healthcare providers.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign provider enrollment faqs

Edit your provider enrollment faqs form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your provider enrollment faqs form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing provider enrollment faqs online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit provider enrollment faqs. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
With pdfFiller, it's always easy to work with documents.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
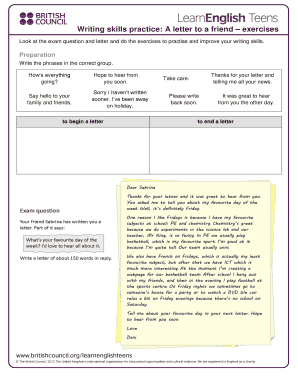
How to fill out provider enrollment faqs

How to fill out Provider Enrollment FAQs
01
Gather all necessary documents related to the provider's qualifications and licenses.
02
Visit the provider enrollment webpage of the relevant healthcare program or insurance company.
03
Locate the FAQs section on the webpage.
04
Read through the FAQs carefully to understand common questions and answers.
05
Identify any specific sections that pertain directly to your situation or specialty.
06
Take notes on key points and gather additional information as needed.
07
Fill out the required sections in the Provider Enrollment application based on the insights gained from the FAQs.
08
Review the completed application for accuracy and completeness before submission.
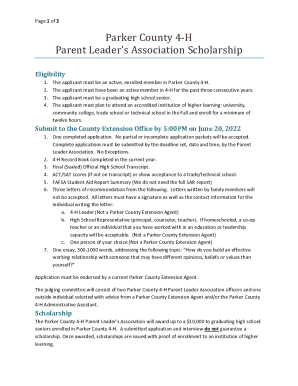
Who needs Provider Enrollment FAQs?
01
Healthcare providers seeking enrollment in insurance plans or government programs.
02
Administrators responsible for managing provider enrollment processes.
03
Billing specialists who need to understand requirements for claims processing.
04
New providers looking for guidance on the enrollment process.
05
Staff assisting providers with their applications for enrollment.
Fill
form
: Try Risk Free






People Also Ask about
Is payer enrollment licensing or credentialing?
While credentialing is the process to certify a provider's qualifications to practice medicine, payer enrollment is the process of requesting participation in a health plan network, including commercial payers such as Humana and Aetna and government programs such as Medicare and Medicaid.
What comes first, credentialing or privileging?
Hospitals and other health care employers and payers both have credentialing processes to complete. Credentialing is closely tied with privileging and is frequently a first step for physicians seeking hospital privileges.
What are the three types of credentialing?
What is an Example of Credentialing? Professional Credentialing. Facility Credentialing. Payer Enrollment Credentialing.
What is the purpose of provider enrollment?
Most insurance companies and government payers, like Medicare, require providers to be enrolled before they can submit claims. Being in-network can bring in new patients and secure better reimbursement rates. On the other hand, failure to enroll can mean providers can't submit claims to certain payers.
Why is provider enrollment important?
Medicare typically completes enrollment applications in 60 – 90 days.
What's the difference between credentialing and provider enrollment?
Why Is Provider Enrollment Important? Provider enrollment allows providers to join the insurance plans accepted by their healthcare organization or practice. It's also a legal requirement. Most insurance companies and government payers, like Medicare, require providers to be enrolled before they can submit claims.
What is the provider enrollment process?
Provider Enrollment (or Payor Enrollment) refers to the process of applying to health insurance networks for inclusion in their provider panels. For Commercial Insurance networks, this process involves two steps, 1) Credentialing and 2) Contracting.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Provider Enrollment FAQs?
Provider Enrollment FAQs are a set of frequently asked questions and answers that help providers understand the enrollment process required to participate in health care programs.
Who is required to file Provider Enrollment FAQs?
Healthcare providers who wish to participate in programs such as Medicare and Medicaid are required to file Provider Enrollment FAQs.
How to fill out Provider Enrollment FAQs?
To fill out Provider Enrollment FAQs, providers should carefully read each question, provide accurate information, and follow the specific instructions outlined in the enrollment forms.
What is the purpose of Provider Enrollment FAQs?
The purpose of Provider Enrollment FAQs is to clarify the enrollment process, provide guidance on required documentation, and address common concerns and questions from healthcare providers.
What information must be reported on Provider Enrollment FAQs?
Providers must report information such as their professional qualifications, practice locations, patient populations served, and any relevant legal or disciplinary history.
Fill out your provider enrollment faqs online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Provider Enrollment Faqs is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.