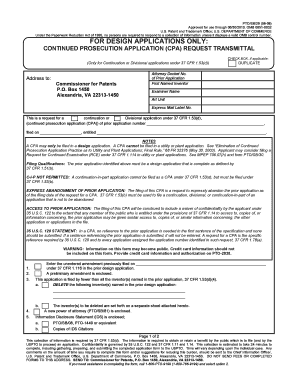
Get the free Utilization Review Programs Certification of Compliance - insurance ohio
Show details
This document certifies that a Health Insuring Corporation has implemented a Utilization Review Program in compliance with relevant sections of the Ohio Revised Code, detailing operational procedures
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign utilization review programs certification
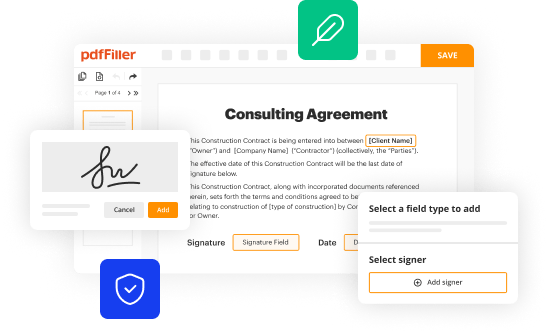
Edit your utilization review programs certification form online
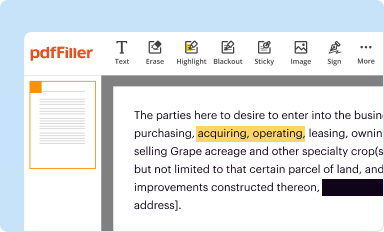
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
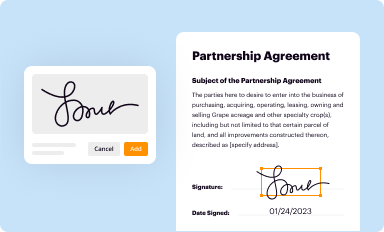
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
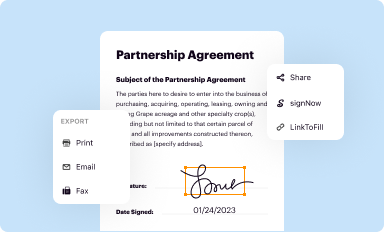
Share your form instantly
Email, fax, or share your utilization review programs certification form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing utilization review programs certification online
Use the instructions below to start using our professional PDF editor:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit utilization review programs certification. Text may be added and replaced, new objects can be included, pages can be rearranged, watermarks and page numbers can be added, and so on. When you're done editing, click Done and then go to the Documents tab to combine, divide, lock, or unlock the file.
4
Save your file. Select it from your list of records. Then, move your cursor to the right toolbar and choose one of the exporting options. You can save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud, among other things.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out utilization review programs certification
How to fill out Utilization Review Programs Certification of Compliance
01
Obtain the Utilization Review Programs Certification of Compliance form from the relevant authority or website.
02
Read the instructions carefully to understand all the requirements for completion.
03
Fill out your organization's details, including name, address, and contact information.
04
Describe your utilization review program, including its structure, processes, and objectives.
05
Provide documentation that demonstrates compliance with relevant regulations and standards.
06
Include any supporting evidence, such as training materials or policy documents.
07
Review the completed form for accuracy and completeness before submission.
08
Submit the form along with any required fees to the appropriate regulatory body.
Who needs Utilization Review Programs Certification of Compliance?
01
Health care organizations that conduct utilization review activities.
02
Health insurance companies looking to comply with state or federal regulations.
03
Providers seeking accreditation for their utilization review programs.
Fill
form
: Try Risk Free






People Also Ask about
What are the three steps in utilization review?
Reviews happen in these three stages: Prospective: In this stage, a patient seeks approval in preparation for care. Concurrent: Reviews take place during care to evaluate medical necessity. Retrospective: This review evaluates after-care plans including outpatient therapies.
What are the three activities within the utilization review process?
Utilization review: Utilization review determines the appropriateness of the prescribed treatment plan to ensure a high quality of care and prevent unnecessary procedures. It is broken down into three phases of review: prospective, concurrent, and retrospective.
What are the three types of utilization review?
Many employers prefer utilization review specialists who have an associate or a bachelor's degree in a medical or health-related field, though some may consider candidates without a degree who have extensive experience in medical billing and health care quality assurance roles.
How do I get a utilization certificate?
Utilization Certificate to be signed by the Chief Finance Officer (Head of the Finance) and Head of the Organisation, as specified on Form GFR 12-A. Project-wise expenditure and physical progress to be attached by SMCG/Executing Agency(s) with Utilization Certificate in the following format.
What are the 3 assessments for utilization management?
Types of UM: Prior Authorization. The prior authorization, or pre-auth, is done before a clinical intervention is delivered. Concurrent Review. The concurrent review takes place while the patient is receiving care while admitted to a facility. Retrospective Review.
What are the three categories of utilization review?
There are three types of utilization reviews: Prospective review: determines whether services or scheduled procedures are medically necessary before admission. Concurrent review: evaluates medical necessity decisions during hospitalization. Retrospective review: examines coverage after treatment.
How to become a utilization review specialist?
Do you get a good deal as a Utilization Review Nurse ? StateAnnual SalaryHourly Wage California $86,795 $41.73 Minnesota $86,136 $41.41 Rhode Island $86,127 $41.41 New Hampshire $85,529 $41.1261 more rows
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Utilization Review Programs Certification of Compliance?
Utilization Review Programs Certification of Compliance is a formal declaration that an organization’s utilization review processes meet the established standards set by regulatory bodies, ensuring that healthcare services provided are necessary and appropriate.
Who is required to file Utilization Review Programs Certification of Compliance?
Healthcare organizations that conduct utilization review activities, such as insurance companies and managed care organizations, are typically required to file the Utilization Review Programs Certification of Compliance.
How to fill out Utilization Review Programs Certification of Compliance?
To fill out the Utilization Review Programs Certification of Compliance, provide accurate information about the organization’s utilization review processes, confirm adherence to compliance standards, and submit the required supporting documentation as stipulated by the regulatory authority.
What is the purpose of Utilization Review Programs Certification of Compliance?
The purpose of Utilization Review Programs Certification of Compliance is to ensure that healthcare services are delivered effectively, efficiently, and in accordance with legal standards, thereby safeguarding patient care and optimizing resource utilization.
What information must be reported on Utilization Review Programs Certification of Compliance?
The information that must be reported includes the organization’s name, contact information, the details of the utilization review program, compliance with regulatory standards, and any relevant performance metrics or outcomes related to the review process.
Fill out your utilization review programs certification online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Utilization Review Programs Certification is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.