Get the free Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries - dhrm vir...
Show details
This document provides details on the annual Open Enrollment period for Extended Coverage/COBRA qualified beneficiaries of the Virginia Health Benefits Program, including plan options, changes, premium
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign open enrollment guide for
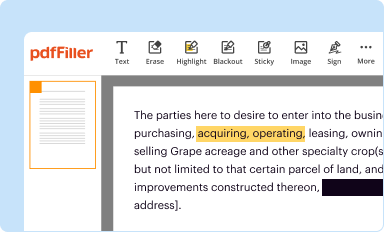
Edit your open enrollment guide for form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
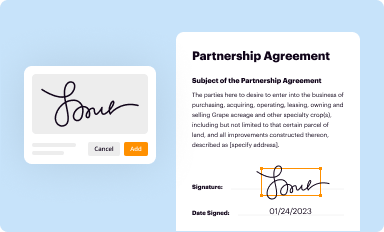
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your open enrollment guide for form via URL. You can also download, print, or export forms to your preferred cloud storage service.
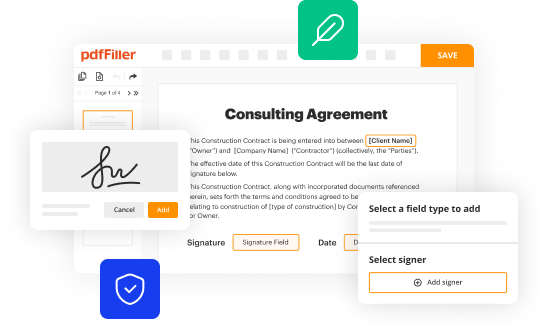
Editing open enrollment guide for online
Follow the steps down below to benefit from the PDF editor's expertise:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit open enrollment guide for. Text may be added and replaced, new objects can be included, pages can be rearranged, watermarks and page numbers can be added, and so on. When you're done editing, click Done and then go to the Documents tab to combine, divide, lock, or unlock the file.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
It's easier to work with documents with pdfFiller than you can have ever thought. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out open enrollment guide for
How to fill out Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries
01
Obtain the Open Enrollment Guide from your employer or the plan administrator.
02
Review the eligibility criteria for Extended Coverage/COBRA to confirm your qualification.
03
Carefully read through the instructions provided in the guide.
04
Complete the application form included in the guide, ensuring all required fields are filled.
05
Gather any necessary documentation, such as proof of previous coverage and personal identification.
06
Make a copy of the completed application and documentation for your records.
07
Submit the application and required documents to the appropriate contact as specified in the guide.
08
Keep an eye out for confirmation of your enrollment or any additional communication from the plan administrator.
Who needs Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries?
01
Individuals who have recently lost their health coverage due to employment termination or reduction in work hours.
02
Dependents of employees who are eligible for Extended Coverage under COBRA.
03
Individuals who want to ensure continued health insurance during a transition between jobs.
Fill
form
: Try Risk Free






People Also Ask about
What is a qualifying beneficiary?
Qualified Beneficiaries can include: Spouses of employees who were covered under the employer's health insurance plan. Dependent children who were covered under the employer's health insurance plan.
Do COBRA participants go through open enrollment?
You should receive an Open Enrollment notification that will provide you with a breakdown of available plans from which you can elect.
What is a qualifying event to extend COBRA?
How Long Can You Stay On COBRA? Qualifying COBRA EventLength of Continuation Coverage Involuntary Termination of Employment (getting fired from job) 18 Months Divorce, Annulment, Termination of Domestic Partnership, or Legal Separation 36 Months Child ceases to be a Dependent (e.g. child turns 26) 36 Months3 more rows
Who are the qualified beneficiaries?
“Qualified beneficiary” means a living beneficiary who, on the date the beneficiary's qualification is determined: (a) Is a distributee or permissible distributee of trust income or principal; (b) Would be a distributee or permissible distributee of trust income or principal if the interests of the distributees
Who is considered a qualified beneficiary under COBRA?
A qualified beneficiary is an individual who is entitled to COBRA continuation coverage because he or she was covered by a group health plan on the day before a “qualifying event.” Depending on the circumstances, the following individuals may be qualified beneficiaries: a "covered employee" (a term that includes active
Who are qualified beneficiaries under COBRA?
A qualified beneficiary is an individual who is entitled to COBRA continuation coverage because he or she was covered by a group health plan on the day before a “qualifying event.” Depending on the circumstances, the following individuals may be qualified beneficiaries: a "covered employee" (a term that includes active
What is the 60 day COBRA loophole?
You have 60 days to enroll in COBRA once your employer-sponsored benefits end. Even if your enrollment is delayed, you will be covered by COBRA starting the day your prior coverage ended.
What are examples of individuals who would qualify for COBRA?
Only certain individuals can become qualified beneficiaries due to a qualifying event, and the type of qualifying event determines who can become a qualified beneficiary when it happens. A qualified beneficiary must be a covered employee, the employee's spouse or former spouse, or the employee's dependent child.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries?
The Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries is a document that outlines the options and procedures for individuals who are eligible for COBRA continuation coverage. It provides information about the rights of qualified beneficiaries to maintain their health insurance coverage after certain qualifying events.
Who is required to file Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries?
Employers with 20 or more employees are required to file the Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries to inform eligible employees and their dependents of their rights to COBRA coverage.
How to fill out Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries?
To fill out the Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries, individuals need to provide personal information, including the covered employee's details, qualifying event information, and any chosen coverage options. It’s essential to follow the instructions carefully and submit the form within the designated time frame.
What is the purpose of Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries?
The purpose of the Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries is to communicate the rights and options available to qualified beneficiaries regarding their health insurance coverage after a qualifying event, ensuring they understand how to maintain their benefits.
What information must be reported on Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries?
The information that must be reported on the Open Enrollment Guide for Extended Coverage/COBRA Qualified Beneficiaries typically includes the covered employee's name, details about the qualifying event, the type of coverage options available, and the deadlines for enrollment and payment.
Fill out your open enrollment guide for online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Open Enrollment Guide For is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.