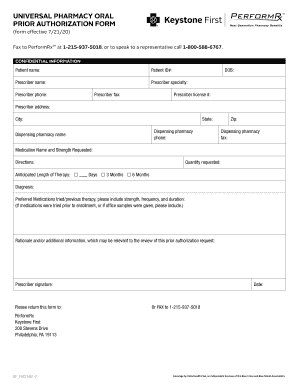
Keystone First Universal Pharmacy Oral Prior Authorization Form 2010 free printable template
Get, Create, Make and Sign Keystone First Universal Pharmacy Oral Prior
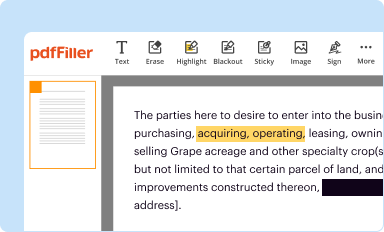
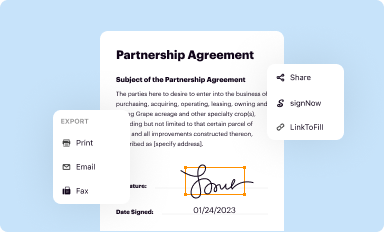
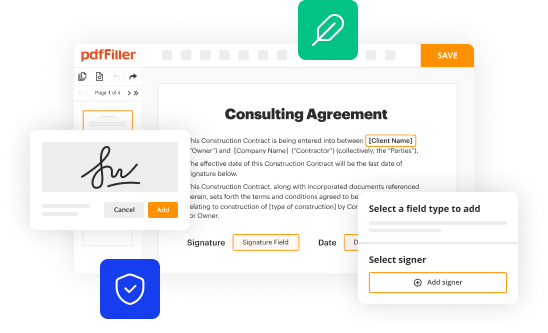
Editing Keystone First Universal Pharmacy Oral Prior online
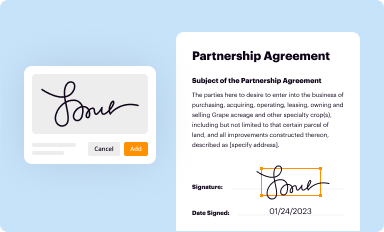
Uncompromising security for your PDF editing and eSignature needs
Keystone First Universal Pharmacy Oral Prior Authorization Form Form Versions
How to fill out Keystone First Universal Pharmacy Oral Prior
How to fill out Keystone First Universal Pharmacy Oral Prior Authorization
Who needs Keystone First Universal Pharmacy Oral Prior Authorization?
Instructions and Help about Keystone First Universal Pharmacy Oral Prior
You and your doctor have selected a new medicine to treat your condition you'rerelieved you×39’re hopintreatmentnt willll work better than the last anyone×39’re hoping that it wilimproviseruqualityty of life, but before you can fill your prescription or have it administered in the doctor's office you may need your health plans approval×39’s a process knowprioroauthorizationonon prior authorization may require your doctor to submit paperwork along with your lab results and record sit can be a multi-step process if the health insurer finds an error in the paperwork are determines that you don'ttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttttmeet their requirements they can deny the request you and your physician can appeal, but the insurer may deny your request again the process can block access to your medication for days even weeks prior authorization is intended to stop unnecessary use of costly drugs but for health plans that has become a tool for cutting expenses especially for innovative drugs like biologics for doctors and other health care providers×39’s a drain on time and resources andistractionon from patient care and for patients like you, it's a delay that cane frustrating even dangers consider patients with chronic conditions such as severe asthma eczema our high cholesterol waiting for the medication or device they need can leave them untreated and unprotected in many cases the insurer finally approves the treatment but some patients simply done×39;have the time or the energy to fight through a multi-step approval in denial process especially when they're ill they may give up on treatment all together using delays and denials to block patients access to their prescribed medications cuts cost at patients expense some state lawmakers have introduced legislation to putcommon-sense limits on prior authorization these efforts are important for patient access limiting burdensome prior authorization can help restore you and your doctors ability to make personalized health care decisions ensuring that the doctor-patientrelationship not help plan cost-cuttingdetermines your course of treatment you Music






People Also Ask about
How do I write a prior authorization request?
How can I make my prior authorization easier?
Why is it so hard to get a prior authorization?
Can you speed up a prior authorization?
Does Keystone First require prior authorization?
What is the phone number for Keystone First Medicaid prior authorization?
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my Keystone First Universal Pharmacy Oral Prior in Gmail?
Can I sign the Keystone First Universal Pharmacy Oral Prior electronically in Chrome?
How do I edit Keystone First Universal Pharmacy Oral Prior on an Android device?
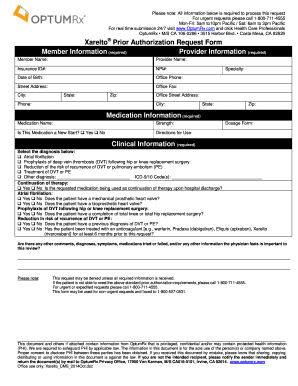
What is Keystone First Universal Pharmacy Oral Prior Authorization?
Who is required to file Keystone First Universal Pharmacy Oral Prior Authorization?
How to fill out Keystone First Universal Pharmacy Oral Prior Authorization?
What is the purpose of Keystone First Universal Pharmacy Oral Prior Authorization?
What information must be reported on Keystone First Universal Pharmacy Oral Prior Authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.