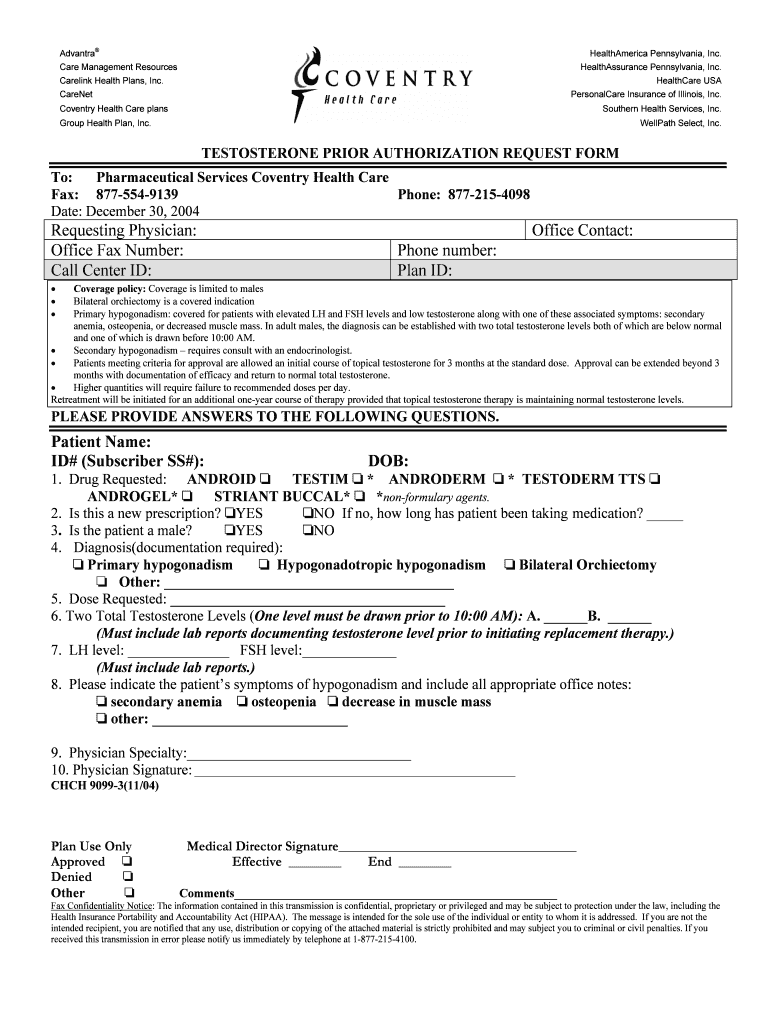
Get the free TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM
Show details
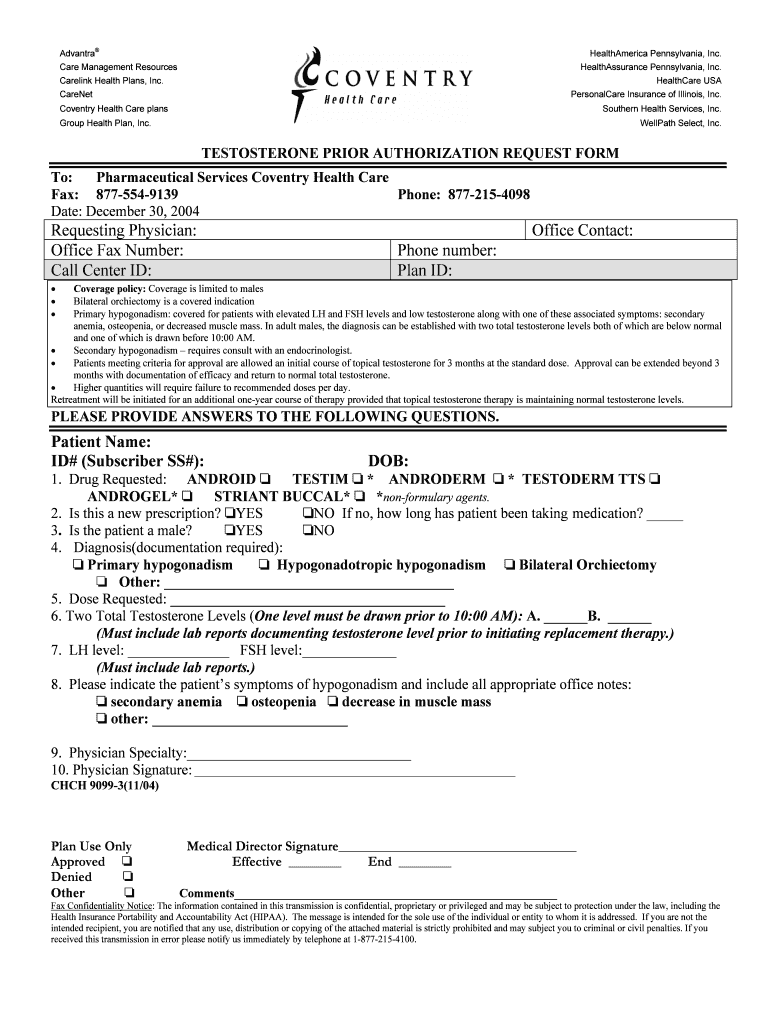
This form is used by healthcare providers to request prior authorization for testosterone therapy for male patients, including medical details required for approval.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign testosterone prior authorization request
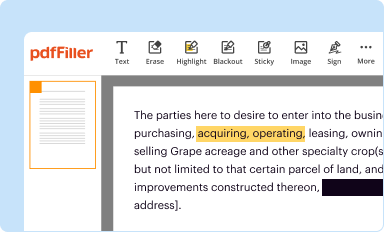
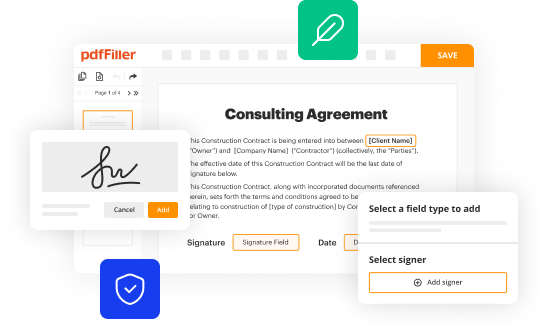
Edit your testosterone prior authorization request form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your testosterone prior authorization request form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit testosterone prior authorization request online
To use our professional PDF editor, follow these steps:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit testosterone prior authorization request. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
It's easier to work with documents with pdfFiller than you can have ever thought. Sign up for a free account to view.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out testosterone prior authorization request
How to fill out TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM
01
Obtain the TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM from your healthcare provider or the insurance company's website.
02
Fill out patient information, including full name, date of birth, and insurance details.
03
Provide details about the prescribing physician, including their name, contact information, and National Provider Identifier (NPI) number.
04
Indicate the type of testosterone therapy being requested, including dosage and form (injection, gel, etc.).
05
Include relevant medical history, including diagnosis, previous treatments, and ongoing medications.
06
Attach supporting documents such as lab results, medical records, or clinical notes that justify the need for testosterone therapy.
07
Review the form for completeness and accuracy before submission.
08
Submit the completed form to the insurance company via the preferred method (fax, mail, or online).
09
Follow up with the insurance company to confirm receipt and ask about the timeline for approval.
Who needs TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM?
01
Individuals diagnosed with low testosterone levels (hypogonadism) who require testosterone replacement therapy.
02
Patients experiencing symptoms of low testosterone, such as fatigue, depression, or reduced libido, who are seeking treatment.
03
Men with specific medical conditions that lead to testosterone deficiency and need therapy to improve their health and well-being.
Fill
form
: Try Risk Free






People Also Ask about
How do I get my doctor to prescribe testosterone?
Doctors prescribe testosterone replacement therapy (TRT) to treat testosterone deficiency (TD). To qualify for TRT, a person needs to get diagnosed with TD. The doctor can then prescribe injectable testosterone therapy.
How do you get prescribed testosterone boosters?
You need a prescription from your doctor to access testosterone. But even if your doctor finds out that your testosterone levels are low, they may want you to try other remedies first – for instance, losing weight or seeing a psychologist for depression – before prescribing testosterone.
What does a prior authorization form do?
Prior authorization requires your doctor or provider to obtain approval from your health plan before providing health care services or prescribing prescription drugs. Without prior authorization, your health plan may not pay for your treatment or medication.
What is a prior authorization request form?
Prior Authorizations Under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care. Prior authorization is usually required if you need a complex treatment or prescription. Coverage will not happen without it.
What happens if you don't get prior authorization?
What is a prior authorization? Insurance companies use prior authorizations to determine medical necessity before a patient's treatment can begin. A prior authorization can be required for anything from prescription drugs to life-saving surgeries.
Does testosterone require prior authorization?
All requests for Testosterone Supplementation require a Prior Authorization and will be screened for medical necessity and appropriateness using the criteria listed below.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM?
The Testosterone Prior Authorization Request Form is a document that healthcare providers use to obtain approval from insurance companies or payers before prescribing testosterone therapy to patients.
Who is required to file TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM?
Healthcare providers, such as physicians or specialists, are typically required to file the Testosterone Prior Authorization Request Form on behalf of their patients to ensure that the therapy is covered by insurance.
How to fill out TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM?
To fill out the Testosterone Prior Authorization Request Form, healthcare providers need to provide patient information, details about the medical necessity for testosterone therapy, previous treatment history, and any relevant lab results.
What is the purpose of TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM?
The purpose of the Testosterone Prior Authorization Request Form is to ensure that treatments are medically necessary and to manage costs associated with testosterone therapy, allowing for insurance approval before treatment begins.
What information must be reported on TESTOSTERONE PRIOR AUTHORIZATION REQUEST FORM?
The information that must be reported includes patient demographics, prescription details, diagnosis codes, previous therapy used, lab results showing testosterone levels, and the rationale for needing the treatment.
Fill out your testosterone prior authorization request online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Testosterone Prior Authorization Request is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.