
Get the free First Choice Pharmacy Benefit Guide
Show details
This document provides detailed information about the UPMC Health Plan's First Choice pharmacy program, including covered medications, formularies, prior authorization processes, and network pharmacy
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign first choice pharmacy benefit
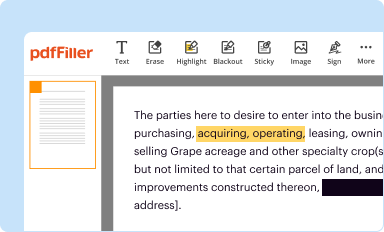
Edit your first choice pharmacy benefit form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
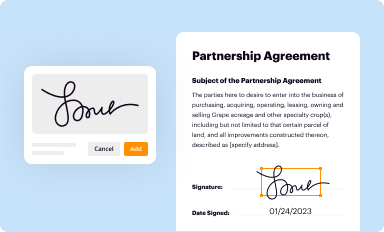
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
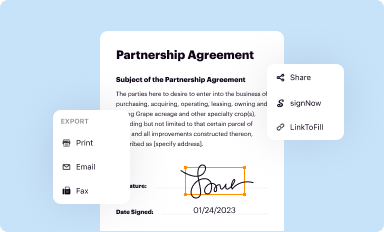
Share your form instantly
Email, fax, or share your first choice pharmacy benefit form via URL. You can also download, print, or export forms to your preferred cloud storage service.
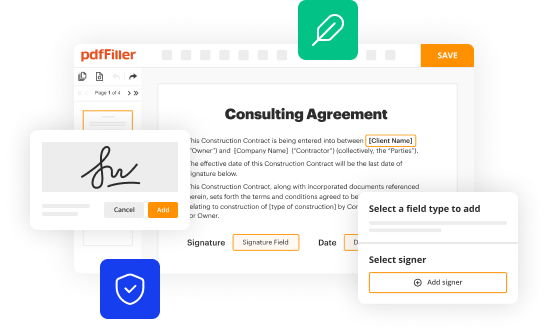
Editing first choice pharmacy benefit online
Use the instructions below to start using our professional PDF editor:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit first choice pharmacy benefit. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Save your file. Select it from your list of records. Then, move your cursor to the right toolbar and choose one of the exporting options. You can save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud, among other things.
pdfFiller makes dealing with documents a breeze. Create an account to find out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out first choice pharmacy benefit
How to fill out First Choice Pharmacy Benefit Guide
01
Obtain a copy of the First Choice Pharmacy Benefit Guide.
02
Read through the introduction to understand the purpose of the guide.
03
Locate the section for personal information and fill in your name, address, and contact details.
04
Provide your insurance information, including policy number and provider details.
05
Review the list of covered medications and mark any that you regularly take.
06
Fill out any required disclosures or consent forms included in the document.
07
Check for specific instructions regarding submission methods (such as mail, fax, or online submission).
08
Ensure all sections are completed and review for accuracy.
09
Submit the form according to the provided instructions.
Who needs First Choice Pharmacy Benefit Guide?
01
Individuals enrolled in a health plan that includes First Choice Pharmacy.
02
Patients who require prescription medications and want to understand their benefits.
03
Caregivers or family members managing medications for others in need of pharmacy benefits.
04
Healthcare providers assisting patients in navigating their pharmacy benefits.
Fill
form
: Try Risk Free






People Also Ask about
What is the difference between pharmacy and medical insurance?
Generally, medical insurance covers care in a hospital or healthcare professional's office, and prescription drug insurance pays for the medications you buy at the pharmacy. There are exceptions. For instance, if you are given medication in the hospital or at your doctor's office, your medical insurance may pay for it.
What is the difference between a pharmacy benefit manager and a specialty pharmacy?
Like specialty pharmacies, PBMs fill prescriptions often via mail and offer specialty pharmacy services. In short, PBMs are generally larger organizations than specialty pharmacies with more complex organizational structures that focus on more than just providing specialty drugs.
What is the difference between medical and pharmacy?
In short, medicine is about the process of the treatment, which includes meeting with patients, diagnosing illnesses and administering treatment. Meanwhile, pharmacy is about the medication that treats patients, ensuring that they are suitable and effective.
What is the difference between a medical benefit and a pharmacy benefit?
This is because when covered under the pharmacy benefit, associated out-of-pocket costs are immediately applied toward the deductible and max out-of-pocket. Under the medical benefit, the claim submitted by the provider's office who administered the drug undergoes review before it is approved.
How do I use my pharmacy insurance?
At the pharmacy, give your insurance card to the pharmacist so they'll know how to bill your insurance company. Depending on your plan, you might have a separate card for prescriptions. You'll usually have to pay part of the bill for your medicines.
What is the difference between a medical claim and a pharmacy claim?
Pharmacy billing occurs when a prescription is sent to the pharmacy to bill a patient's drug insurance, while medical billing occurs when the provider submits the claim to the patient's medical insurance. Sometimes, insurance requires a specific type of billing, but, at other times, the provider can choose.
What are the tiers of pharmacy benefit?
Tier 1: Least expensive drug options, often generic drugs. Tier 2: Higher price generic and lower-price brand-name drugs. Tier 3: Mainly higher price brand-name drugs. Tier 4: Highest cost prescription drugs.
What is pharmacy benefit vs medical benefit?
In the world of health insurance, “It depends” is a common answer to many coverage questions. As previously mentioned, specialty medication is typically covered under the pharmacy benefit if self-injected/self-administered and under the medical benefit when administered by a healthcare provider.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is First Choice Pharmacy Benefit Guide?
The First Choice Pharmacy Benefit Guide is a document that outlines the pharmacy benefits offered by the First Choice insurance plan, including covered medications, co-pays, and the claims process.
Who is required to file First Choice Pharmacy Benefit Guide?
Individuals enrolled in the First Choice insurance plan are required to file the First Choice Pharmacy Benefit Guide to ensure they receive the correct pharmacy benefits and reimbursements.
How to fill out First Choice Pharmacy Benefit Guide?
To fill out the First Choice Pharmacy Benefit Guide, individuals must provide their personal information, details of the pharmacy transaction, including prescription numbers, and any receipts or documentation required for reimbursement.
What is the purpose of First Choice Pharmacy Benefit Guide?
The purpose of the First Choice Pharmacy Benefit Guide is to facilitate the claims process for pharmacy benefits and ensure that members understand their coverage and how to access medications.
What information must be reported on First Choice Pharmacy Benefit Guide?
The information that must be reported on the First Choice Pharmacy Benefit Guide includes patient details, prescription information, pharmacy name, date of service, amount charged, and the member's insurance details.
Fill out your first choice pharmacy benefit online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

First Choice Pharmacy Benefit is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















