
Get the free Medical Staff Progress Notes
Show details
This document provides updates and important information for the Medical Staff of Lehigh Valley Hospital, including articles on medical issues, updates on hospital procedures, and announcements related
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign medical staff progress notes
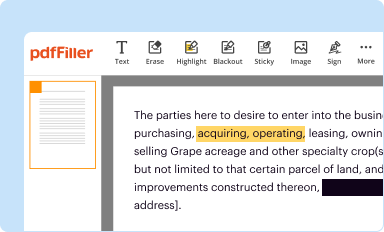
Edit your medical staff progress notes form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
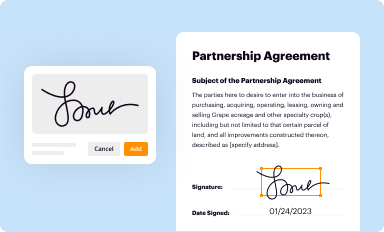
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
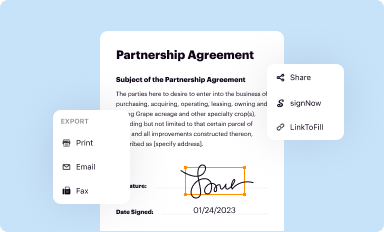
Share your form instantly
Email, fax, or share your medical staff progress notes form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit medical staff progress notes online
Use the instructions below to start using our professional PDF editor:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
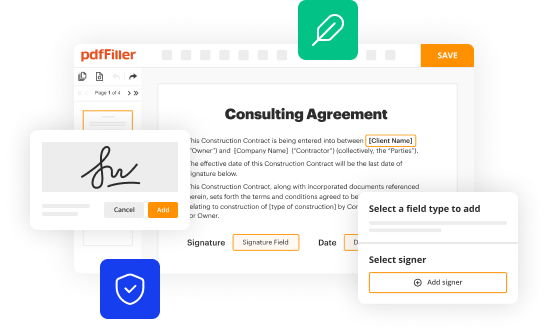
Edit medical staff progress notes. Text may be added and replaced, new objects can be included, pages can be rearranged, watermarks and page numbers can be added, and so on. When you're done editing, click Done and then go to the Documents tab to combine, divide, lock, or unlock the file.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out medical staff progress notes
How to fill out Medical Staff Progress Notes
01
Begin with the patient's basic information such as name, date of birth, and medical record number.
02
Date and time of the entry should be recorded clearly.
03
Provide a brief overview of the patient's current condition and any changes since the last note.
04
Document any assessments made, including vital signs, physical findings, and patient complaints.
05
Include details about the treatment provided during the visit or session, specifying any medications or procedures administered.
06
Note the patient's response to the treatment, including any side effects or improvements.
07
Plan the next steps in treatment, including referrals, additional tests, or follow-up appointments.
08
Conclude with the signature and credentials of the healthcare provider writing the note.
Who needs Medical Staff Progress Notes?
01
Healthcare providers involved in the patient's care, including physicians, nurses, and therapists.
02
Medical coders and billers who need accurate documentation for reimbursement.
03
Insurance companies that require detailed medical records for claims processing.
04
Patients, for their own records and to understand their treatment history.
05
Quality assurance teams that monitor compliance and the effectiveness of care provided.
Fill
form
: Try Risk Free






People Also Ask about
How do you write medical notes?
Good clinical notes should: Clearly outline the patient's medical history, current condition, and treatment plan. Be organized in a logical structure, making it easy to understand. Include objective data, such as vital signs and lab results, alongside subjective information, like patient complaints and observations.
How to write basic patient notes?
What to include in patient notes Presenting complaint and history. Begin by documenting the patient's presenting complaint and relevant medical history. Objective findings. Assessment and diagnosis. Medication management. Follow-up plan and monitoring.
How to write a medical progress note?
Progress notes should outline the evidence-based practice used in the session, and comment on any changes in modality. You might also include any skills that may be helpful for clients to practice to help manage or reduce their symptoms, and why it would be helpful in reducing their symptoms.
How to write medical notes example?
Good clinical notes should: Clearly outline the patient's medical history, current condition, and treatment plan. Be organized in a logical structure, making it easy to understand. Include objective data, such as vital signs and lab results, alongside subjective information, like patient complaints and observations.
What is the preferred format for medical notes?
The order in which a medical note is written has been a topic of discussion. While a SOAP note follows the order Subjective, Objective, Assessment, and Plan, it is possible, and often beneficial, to rearrange the order.
How to write good nursing progress notes?
How to Write Excellent Nursing Progress Notes Use a Template. Nursing progress notes templates will help you to produce more complete documentation. Write Your Progress Notes Straight Away. Provide Details. Be Concise. Double-Check Your Notes Are Accurate. Use Professional and Objective Language. Adopt the Active Voice.
What is an example of a progress note?
An example of a progress note is: “Attended service at 0900 to provide a personal care service. Client John Doe was in bed on my arrival. I picked up all the laundry for the wash, put away the dishes, and went to wake John at 0915 for his 0930 medication.
What are the five C's in medical record documentation?
5 C's of Clinical Documentation Clarity. Clarity is one of the most essential components of clinical documentation. Conciseness. Medical records should be created in a manner that they are easily digestible to everyone who reads them. Completeness. Confidentiality. Chronological Order.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Medical Staff Progress Notes?
Medical Staff Progress Notes are documentation that provides a continuous record of a patient's clinical status and responses to treatment within a healthcare setting.
Who is required to file Medical Staff Progress Notes?
Typically, licensed healthcare professionals such as physicians, nurse practitioners, and clinical staff are required to file Medical Staff Progress Notes.
How to fill out Medical Staff Progress Notes?
To fill out Medical Staff Progress Notes, the clinician should document the date and time of the encounter, observations, patient status, interventions, and any changes in the treatment plan clearly and succinctly.
What is the purpose of Medical Staff Progress Notes?
The purpose of Medical Staff Progress Notes is to ensure continuity of care, provide legal documentation, facilitate communication among care team members, and support quality assurance and risk management activities.
What information must be reported on Medical Staff Progress Notes?
Medical Staff Progress Notes must report relevant patient information, including the patient's condition, treatment provided, response to treatment, any new symptoms, and plans for future care.
Fill out your medical staff progress notes online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Medical Staff Progress Notes is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.




















