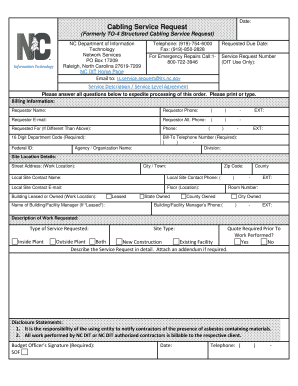
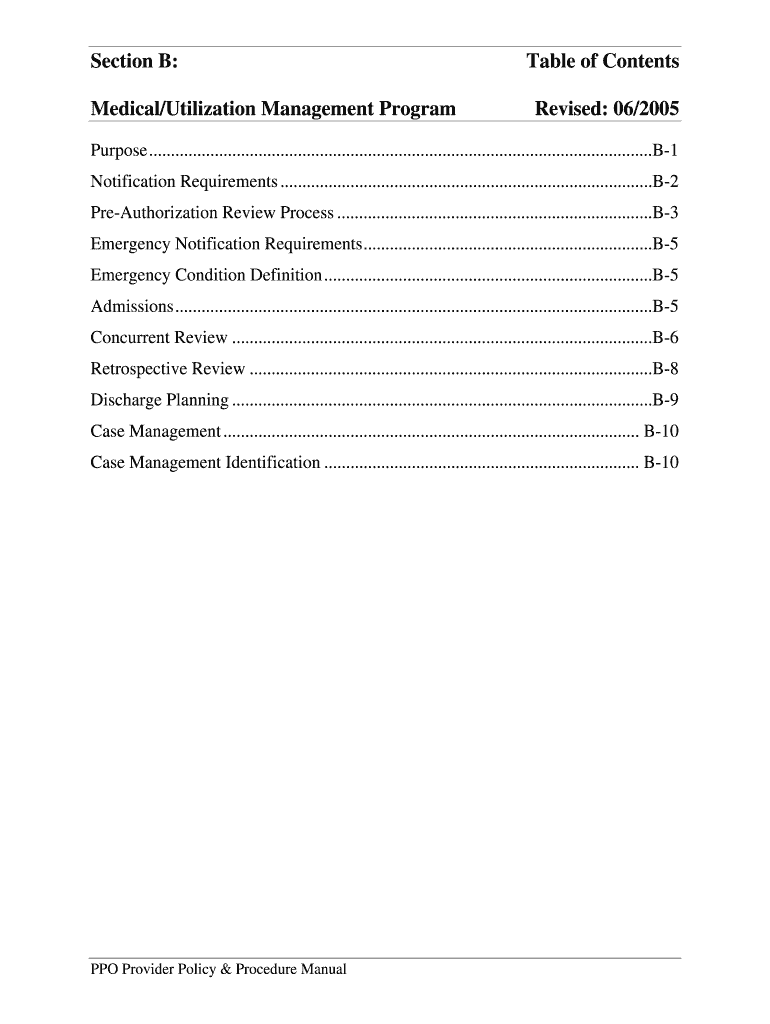
Get the free Medical/Utilization Management Program
Show details
This document outlines the Medical Management/Utilization Management (MM/UM) Program by PacifiCare, detailing requirements for pre-authorization, concurrent reviews, discharge planning, and case management
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign medicalutilization management program
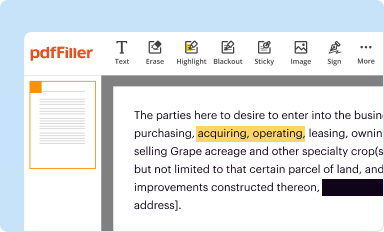
Edit your medicalutilization management program form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your medicalutilization management program form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing medicalutilization management program online
Follow the steps down below to take advantage of the professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit medicalutilization management program. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out medicalutilization management program
How to fill out Medical/Utilization Management Program
01
Gather all relevant patient information and documentation.
02
Review the medical necessity criteria.
03
Complete the required forms accurately, ensuring all sections are filled out.
04
Provide supporting documentation such as test results or prior treatment plans.
05
Submit the completed forms to the designated department or portal.
06
Follow up to confirm receipt and check the status of the request.
Who needs Medical/Utilization Management Program?
01
Healthcare providers seeking approval for specific treatments or procedures.
02
Patients enrolled in insurance plans requiring prior authorization.
03
Organizations aiming to manage and optimize healthcare resources and costs.
Fill
form
: Try Risk Free






People Also Ask about
What are the basic three components of utilization management?
There are three activities within the utilization review process: prospective, concurrent and retrospective.
What are the three basic categories of utilization management?
There are three types of utilization reviews: Prospective review: determines whether services or scheduled procedures are medically necessary before admission. Concurrent review: evaluates medical necessity decisions during hospitalization. Retrospective review: examines coverage after treatment.
What are the three important functions of utilization management?
Definition/Introduction Prior Authorization. The prior authorization, or pre-auth, is done before a clinical intervention is delivered. Concurrent Review. The concurrent review takes place while the patient is receiving care while admitted to a facility. Retrospective Review.
What are three important functions of utilization management?
There are three main types of utilization management: prospective, concurrent, and retrospective reviews. Payers use these reviews to assess services before they are administered, during the treatment course, and after the treatment is completed.
What is a utilization management program?
Utilization management is "a set of techniques used by or on behalf of purchasers of health care benefits to manage health care costs by influencing patient care decision-making through case-by-case assessments of the appropriateness of care prior to its provision," as defined by the Institute of Medicine Committee on
What are examples of UM rules?
Three common examples of UM are requiring prior authorization to fill a prescription, limiting quantities, and requiring consumers to first try a less expensive medication (called step therapy).
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Medical/Utilization Management Program?
A Medical/Utilization Management Program is a systematic approach used by healthcare organizations to assess the necessity, appropriateness, and efficiency of healthcare services and procedures. It aims to ensure patients receive necessary care while controlling costs.
Who is required to file Medical/Utilization Management Program?
Healthcare providers, insurance companies, and healthcare organizations that manage patient care and are involved in the reimbursement process are typically required to file a Medical/Utilization Management Program.
How to fill out Medical/Utilization Management Program?
To fill out a Medical/Utilization Management Program, providers must collect relevant patient data, assess medical necessity using clinical guidelines, document findings, and submit the required forms as per the guidelines of the managing authority or insurance plan.
What is the purpose of Medical/Utilization Management Program?
The purpose of the Medical/Utilization Management Program is to improve the quality of care, ensure appropriate utilization of healthcare resources, reduce unnecessary expenditures, and enhance patient outcomes through informed decision-making.
What information must be reported on Medical/Utilization Management Program?
Information that must be reported typically includes patient demographics, clinical information, reasons for service requests, treatment plans, medical necessity criteria used, and any reviews or denials related to care provision.
Fill out your medicalutilization management program online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Medicalutilization Management Program is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.