Get the free HISTORY & PHYSICAL
Show details
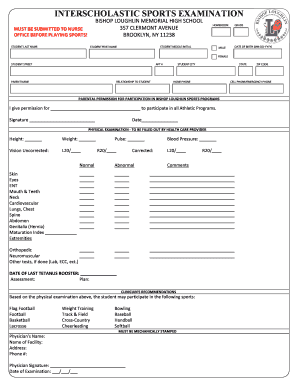
This document is a comprehensive history and physical examination form used for collecting patient information, including personal, medical, family histories, and review of systems. It gathers data
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign history physical

Edit your history physical form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your history physical form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit history physical online
In order to make advantage of the professional PDF editor, follow these steps below:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit history physical. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
With pdfFiller, it's always easy to work with documents.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out history physical

How to fill out HISTORY & PHYSICAL
01
Begin with patient identification: Name, date of birth, and medical record number.
02
Document the chief complaint: The main reason the patient is seeking care.
03
Record the history of present illness: Detailed account of the current condition including onset, duration, and severity.
04
Collect past medical history: Chronic illnesses, previous surgeries, hospitalizations, and relevant treatment outcomes.
05
Note medication history: All current medications, including dosages and durations.
06
Inquire about allergies: Document any known drug, food, or environmental allergies.
07
Gather family history: Significant illnesses in the family that could affect the patient's health.
08
Document social history: Lifestyle factors such as smoking, alcohol use, occupation, and living situation.
09
Conduct a review of systems: Systematic inquiry into each body system to identify any additional concerns.
10
Perform a physical examination: Document vital signs and findings for each body system examined.
11
Summarize findings and plan of care: Include a differential diagnosis and recommended next steps.
Who needs HISTORY & PHYSICAL?
01
Patients scheduled for procedures or surgeries.
02
Patients undergoing annual check-ups.
03
Patients being admitted to hospitals.
04
Patients seeking new medical care or specialists.
05
Patients with chronic conditions requiring routine assessments.
Fill
form
: Try Risk Free






People Also Ask about
Can podiatrists write history and physicals?
The H/P includes considerable more detail and information versus the SOAP note which provides only that information which is relevant to addresses the problem.
What is included in a history and Physical note?
The H&P consists of two parts. The first is a thorough medical history prompted by questions from the practitioner (and any prior medical records that may have been provided). The second portion is the physical exam, which allows the practitioner to assess the patient's current health and address the chief complaint.
What are the components of H and P?
The H&P: History and Physical is the most formal and complete assessment of the patient and the problem. H&P is shorthand for the formal document that physicians produce through the interview with the patient, the physical exam, and the summary of the testing either obtained or pending.
What does a history and Physical include?
The H&P: History and Physical is the most formal and complete assessment of the patient and the problem. H&P is shorthand for the formal document that physicians produce through the interview with the patient, the physical exam, and the summary of the testing either obtained or pending.
What does an H&P consist of?
Can a podiatrist complete an H&P per CMS regulations? ANSWER: Yes. CMS 482.22(c)(5) addresses who may complete a history and physical.
What are the 4 components of a physical exam?
Inspection (looking at the body) Palpation (feeling the body with fingers or hands) Auscultation (listening to sounds, usually with a stethoscope) Percussion (producing sounds, usually by tapping on specific areas of the body)
What should be included in an H&P?
The history component of an H&P gathers relevant information about the patient's history with their current chief complaint. This includes reviewing any pre-existing conditions, past hospitalizations and surgeries, allergies, medications being taken, and family medical history.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is HISTORY & PHYSICAL?
HISTORY & PHYSICAL refers to a comprehensive assessment of a patient's medical history and current physical condition, which is typically documented in a medical record.
Who is required to file HISTORY & PHYSICAL?
HISTORY & PHYSICAL is typically required to be filed by healthcare providers such as physicians, physician assistants, or nurse practitioners before a patient undergoes surgery or other major medical procedures.
How to fill out HISTORY & PHYSICAL?
To fill out a HISTORY & PHYSICAL form, a healthcare provider should gather detailed information about the patient's medical history, current medications, allergies, physical examination findings, and any pertinent diagnostic tests.
What is the purpose of HISTORY & PHYSICAL?
The purpose of HISTORY & PHYSICAL is to gather essential information about a patient's health status to guide treatment decisions, ensure patient safety, and facilitate effective communication among healthcare providers.
What information must be reported on HISTORY & PHYSICAL?
The HISTORY & PHYSICAL must report the patient's past medical history, family health history, social history, a review of systems, physical examination findings, and any relevant laboratory or imaging results.
Fill out your history physical online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

History Physical is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.