Get the free Out-of-Network Claims Questionnaire - slc
Show details
This document serves as a questionnaire for patients to submit out-of-network claims to Health Net, requiring personal and claim-related information.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign out-of-network claims questionnaire
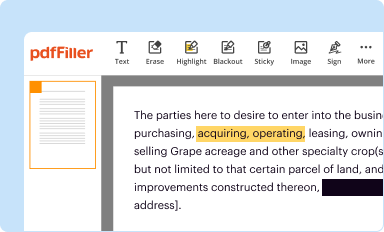
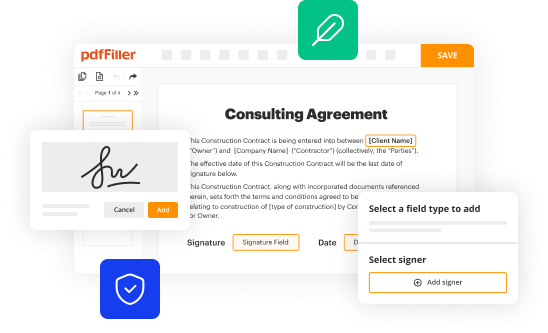
Edit your out-of-network claims questionnaire form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
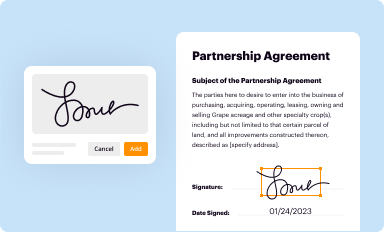
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
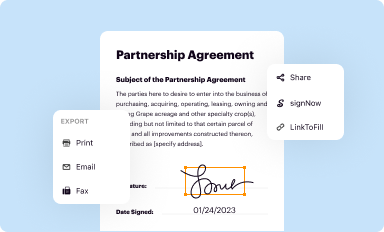
Share your form instantly
Email, fax, or share your out-of-network claims questionnaire form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit out-of-network claims questionnaire online
To use our professional PDF editor, follow these steps:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit out-of-network claims questionnaire. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
With pdfFiller, it's always easy to deal with documents.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
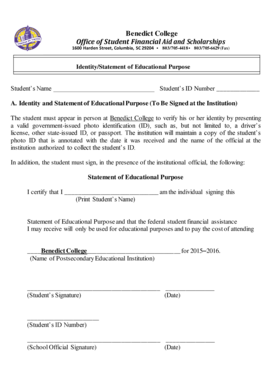
How to fill out out-of-network claims questionnaire
How to fill out Out-of-Network Claims Questionnaire
01
Begin by gathering all necessary documents related to your out-of-network expenses.
02
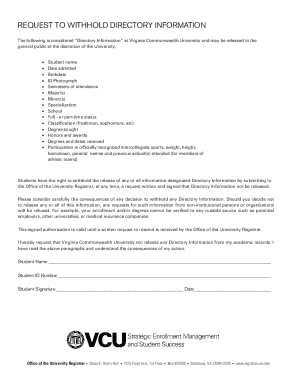
Download or request the Out-of-Network Claims Questionnaire form from your health insurance provider.
03
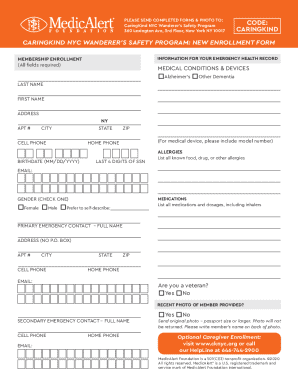
Fill out your personal information at the top of the form, including your name, policy number, and contact information.
04
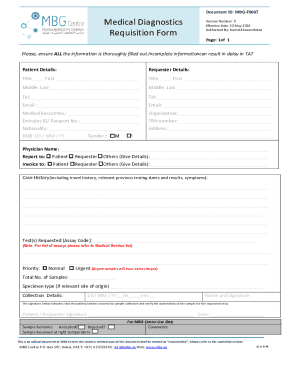
List the healthcare providers you visited, including their names, addresses, and contact information.
05
Detail the services you received during your visits, including dates, types of services, and costs incurred.
06
Attach any supporting documents such as receipts, bills, and medical records to substantiate your claim.
07
Review the completed form to ensure all information is accurate and complete.
08
Submit the questionnaire and accompanying documents to your insurance company as directed, either online or by mail.
09
Keep a copy of all submitted documents for your records.
Who needs Out-of-Network Claims Questionnaire?
01
Individuals who have received medical services from providers outside of their insurance network and wish to claim reimbursement.
02
Patients seeking to understand their out-of-network benefits and how to navigate the claims process.
03
Those who are covered by health insurance plans that include out-of-network options and require a formal process for reimbursement claims.
Fill
form
: Try Risk Free






People Also Ask about
How to get reimbursed for out-of-network therapy?
Receive out-of-network reimbursement! You'll need to pay your therapist the entire session fee at the time of service, but depending on your specific plan, your insurance company will mail you a check to reimburse a portion of that cost. There are even apps for that!
What is out-of-network reimbursement?
Insurance companies usually cover less of the cost of an out-of-network provider. For example, you might have to pay a $25 copay if you see an in-network provider but a $35 copay if you see an out-of-network provider. Insurance companies do not usually reimburse you based on the amount you actually paid your provider.
What is an example of out-of-network?
(They might be in-network with other insurance plans, but they're considered an out-of-network provider if they aren't contracted with your insurance.) So if they bill $160, they'll expect to collect the full $160. Your insurance plan might pay part of the bill if the plan includes out-of-network coverage.
How to submit out of network claims?
For out-of-network providers, the allowed amount is what the insurance company has decided is the usual, customary, and reasonable fee for that service. However, not all insurance plans, like most HMO and EPO plans, cover out-of-network providers.
What is an example of out of network reimbursement?
So, if you visit a therapist who charges $200 per session, and your coinsurance is 20%, you would pay $40 and your insurer would pay the other $160. With both copays and coinsurance, the costs generally increase for out-of-network services, though not as much as you might think.
How to explain out of network benefits to patients?
Your plan allows you to use out of network providers. To submit claims for reimbursement, you must fill out the Health Claim Form and return it along with an itemized statement and proof of payment.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Out-of-Network Claims Questionnaire?
The Out-of-Network Claims Questionnaire is a form used by individuals to provide necessary information about medical services received from healthcare providers that are not part of their insurance network for processing claims.
Who is required to file Out-of-Network Claims Questionnaire?
Individuals who have received medical services from out-of-network providers and wish to file a claim for reimbursement from their insurance are required to fill out the Out-of-Network Claims Questionnaire.
How to fill out Out-of-Network Claims Questionnaire?
To fill out the Out-of-Network Claims Questionnaire, gather all relevant documentation such as invoices and receipts, complete the form by providing required personal and service details, and submit it as per the insurance provider's instructions.
What is the purpose of Out-of-Network Claims Questionnaire?
The purpose of the Out-of-Network Claims Questionnaire is to collect detailed information regarding services received from out-of-network providers to facilitate accurate reimbursement processing by the insurance company.
What information must be reported on Out-of-Network Claims Questionnaire?
The information that must be reported includes patient details, provider information, date and description of services received, total cost, and any relevant insurance policy details.
Fill out your out-of-network claims questionnaire online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Out-Of-Network Claims Questionnaire is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.