Get the free Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion ...
Show details
This document serves to inform employees about their rights regarding enrollment in health care plans under HIPAA, specifically regarding special enrollment provisions and pre-existing condition exclusions.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign initial notice about special
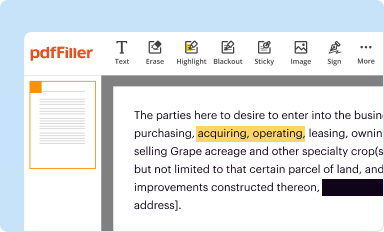
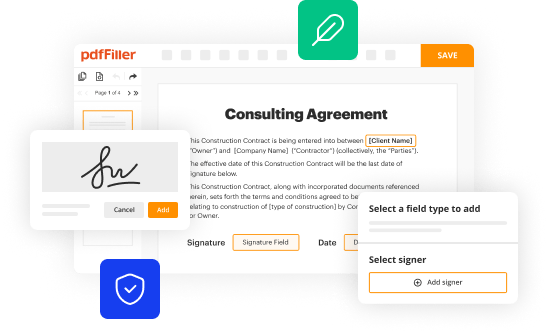
Edit your initial notice about special form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
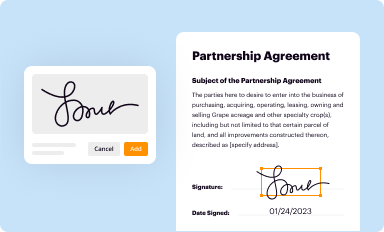
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your initial notice about special form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit initial notice about special online
To use the services of a skilled PDF editor, follow these steps:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit initial notice about special. Text may be added and replaced, new objects can be included, pages can be rearranged, watermarks and page numbers can be added, and so on. When you're done editing, click Done and then go to the Documents tab to combine, divide, lock, or unlock the file.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out initial notice about special
How to fill out Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules in Your Group Health Plan
01
Obtain the Initial Notice from your employer or group health plan administrator.
02
Read through the notice carefully to understand your rights regarding special enrollment and pre-existing conditions.
03
Fill out your personal information including name, address, and contact details as required in the form.
04
Indicate any special enrollment periods you are eligible for, such as due to loss of other health coverage or changes in family status.
05
Acknowledge any pre-existing conditions as outlined in your insurance policy or plan provisions.
06
Submit the completed notice to your employer or plan administrator before the deadline specified in the notice.
Who needs Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules in Your Group Health Plan?
01
Employees who are part of a group health plan.
02
Individuals who are considering enrolling in a health plan and may be impacted by special enrollment rights.
03
Dependents of employees who might need coverage due to changes in eligibility.
04
Anyone who has pre-existing conditions and wants to understand how it affects their enrollment.
Fill
form
: Try Risk Free






People Also Ask about
Which of the following is considered an exceptional condition for the special election period?
"Exceptional circumstances" can be personal – for example, a house fire or a serious medical condition that made it impossible for you to enroll – but they also include natural disasters that impact a large number of people.
Which of the following are examples of situations that could qualify for a special enrollment period?
A change in your situation — like getting married, having a baby, or losing health coverage — that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period. Refer to glossary for more details.
What are the conditions for special enrollment period?
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
What is the purpose of a pre existing condition exclusion on a health insurance policy?
A pre-existing condition exclusion period limits the number of benefits that an insurer has to provide for specific medical conditions and does not apply to medical benefits afforded by a health insurance policy for other types of care.
What is HIPAA special enrollment notice?
Special enrollment allows individuals who previously declined health coverage to enroll for coverage. Special enrollment rights arise regardless of a plan's open enrollment period.
What are the special enrollment events for Hipaa?
If you enroll in COBRA, HIPAA provides you with the opportunity to request special enrollment in a different group health plan if you have a special enrollment event, such as marriage, the birth of a child, or if you exhaust your continuation coverage.
Which of the following is a qualifying event for special enrollment?
Marriage, divorce, and parenthood are all common examples of major qualifying life events that affect a person's health insurance needs. Under these circumstances, an individual qualifies to immediately buy or make changes to a health plan.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules in Your Group Health Plan?
The Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules informs plan participants of their rights regarding special enrollment periods and the rules governing coverage for pre-existing conditions under the group health plan.
Who is required to file Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules in Your Group Health Plan?
Employers or plan sponsors of group health plans are required to provide the Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules to eligible employees and dependents.
How to fill out Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules in Your Group Health Plan?
To fill out the notice, employers should include relevant details such as the eligibility for special enrollment, the circumstances that trigger such enrollment, and a clear explanation of the pre-existing condition exclusion rules applicable to the health plan.
What is the purpose of Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules in Your Group Health Plan?
The purpose of the notice is to educate participants about their rights to enroll in health coverage outside of the open enrollment period and to inform them about the implications of pre-existing condition exclusions.
What information must be reported on Initial Notice About Special Enrollment Rights and Pre-existing Condition Exclusion Rules in Your Group Health Plan?
The notice must report information such as the special enrollment periods, qualifying events that allow for enrollment, details regarding the pre-existing condition exclusion period, and the rights of participants regarding these aspects.
Fill out your initial notice about special online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Initial Notice About Special is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.