
Get the free COBRA VERIFICATION NOTICE - calstate
Show details
This document serves as a verification notice for COBRA (Consolidated Omnibus Budget Reconciliation Act) coverage, detailing the dues payable for continuing health insurance coverage through Blue
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign cobra verification notice
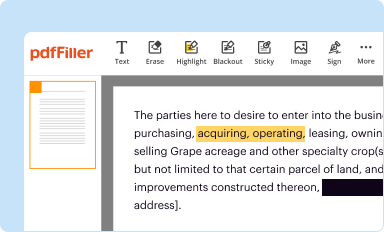
Edit your cobra verification notice form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
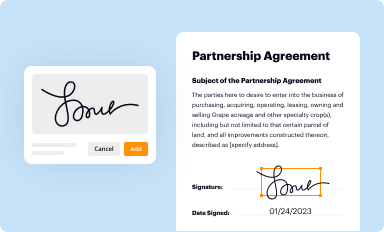
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
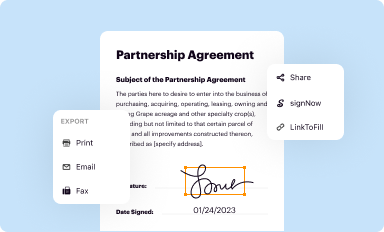
Share your form instantly
Email, fax, or share your cobra verification notice form via URL. You can also download, print, or export forms to your preferred cloud storage service.
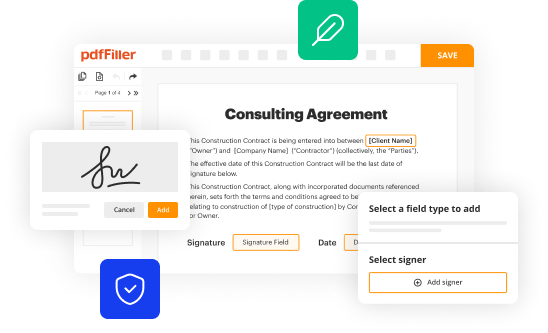
How to edit cobra verification notice online
Follow the steps below to take advantage of the professional PDF editor:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit cobra verification notice. Replace text, adding objects, rearranging pages, and more. Then select the Documents tab to combine, divide, lock or unlock the file.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out cobra verification notice
How to fill out COBRA VERIFICATION NOTICE
01
Begin by identifying the qualifying event that triggers COBRA coverage.
02
Collect the necessary information for the notice, including the name and address of the employer, the name of the plan, and the names of qualified beneficiaries.
03
Clearly state the rights provided by COBRA, including who is eligible for coverage and how long the coverage lasts.
04
Include instructions on how to elect COBRA coverage, including deadlines and where to send the election form.
05
Explain any premium costs and how beneficiaries can pay for coverage.
06
Inform about the consequences of not electing coverage and what steps to take if they have questions.
Who needs COBRA VERIFICATION NOTICE?
01
Employees who have experienced a qualifying event such as termination, reduction in hours, or other life events that affect health insurance coverage.
02
Dependents of employees who are eligible for COBRA coverage due to the employee's qualifying event.
03
Employers who are required to provide the notice to eligible individuals under the COBRA regulations.
Fill
form
: Try Risk Free






People Also Ask about
Why am I getting a letter from COBRA?
As others have noted, this is a general rights notice. Did you recently enroll in your benefits effective May 1st? If so, most companies (mine included) have systems that automatically generate the notice shortly after you enroll in COBRA-eligible benefits (medical, dental, vision, certain FSAs).
What is a COBRA notification letter?
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
How do I verify my COBRA eligibility?
You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
How should COBRA notices be delivered?
COBRA law requires that notices must be furnished to covered individuals. The preferred method of delivery is First Class Mail.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is COBRA VERIFICATION NOTICE?
The COBRA Verification Notice is a document that informs employees and their dependents of their right to continue health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA) after experiencing a qualifying event.
Who is required to file COBRA VERIFICATION NOTICE?
Employers with group health plans that are subject to COBRA regulations are required to provide a COBRA Verification Notice to eligible employees and their dependents.
How to fill out COBRA VERIFICATION NOTICE?
To fill out the COBRA Verification Notice, you must include information such as the qualifying event, the names of eligible individuals, coverage options, and instructions on how to elect COBRA coverage.
What is the purpose of COBRA VERIFICATION NOTICE?
The purpose of the COBRA Verification Notice is to ensure that employees and their dependents are aware of their rights to continued health insurance coverage and the procedures for electing such coverage following a qualifying event.
What information must be reported on COBRA VERIFICATION NOTICE?
The COBRA Verification Notice must report details including the type of qualifying event, the duration of the continuation coverage, the premium amounts, and contact information for the plan administrator.
Fill out your cobra verification notice online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Cobra Verification Notice is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















