Get the free Record of Physical Examination - onu
Show details
A health document required for students at Ohio Northern University's College of Pharmacy that records physical examination details, immunizations, and medical history.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign record of physical examination
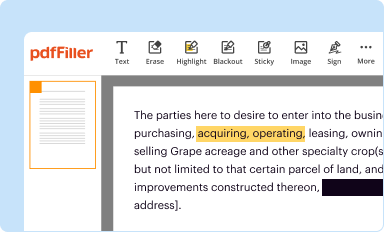
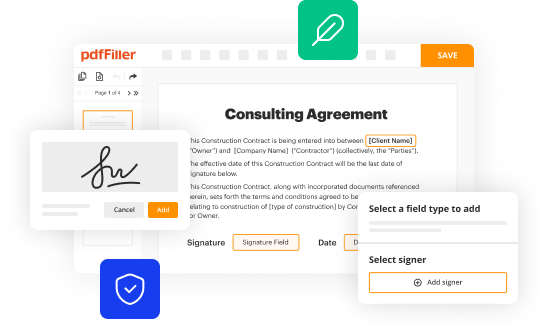
Edit your record of physical examination form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your record of physical examination form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit record of physical examination online
To use the services of a skilled PDF editor, follow these steps:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit record of physical examination. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
It's easier to work with documents with pdfFiller than you could have ever thought. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out record of physical examination
How to fill out Record of Physical Examination
01
Start with the patient's personal information, including name, age, gender, and identification number.
02
Document the date and time of the examination.
03
Include the patient's medical history, including any previous illnesses or surgeries.
04
Record vital signs such as blood pressure, heart rate, respiratory rate, and temperature.
05
Perform a physical assessment, noting any abnormalities in the head, eyes, ears, nose, throat, chest, abdomen, and extremities.
06
Record findings from any laboratory tests or imaging studies if available.
07
Summarize the findings and provide any recommendations for further investigation or treatment.
08
Ensure the record is signed by the examining physician along with their credentials and date.
Who needs Record of Physical Examination?
01
Patients requiring a routine health check-up.
02
Athletes needing a pre-participation examination for sports.
03
Individuals applying for a job that requires a physical examination.
04
Patients seeking insurance coverage that requires proof of physical fitness.
05
People undergoing routine health assessments in schools or workplaces.
Fill
form
: Try Risk Free






People Also Ask about
What is the difference between an H&P and a SOAP note?
Frequently, an H/P is done annually at a given facility while any interim visits for particular health care problems are documented as SOAP notes. Specifically for in-patient settings, after an admission H/P is done, SOAP notes detail the regular follow-up visits by various health care professionals.
What is the difference between a SOAP note and a standard note?
The subjective section should include the history of the present illness, including pertinent positives and negatives. This may be followed by relevant past medical history, family history, social history and/or current medications.
What is the difference between a soap note and H&P?
The HPI should be written in prose with full sentences and be a narrative that builds an argument for the reason the patient was admitted. Has a starting point (i.e. “the patient was in her usual state of health until 5 days prior to admission.). Has appropriate flow, continuity, sequence, and chronologic order.
What is an H&P note?
The primary distinction between a SOAP and Simple note is that the SOAP note has individual sections for the Subjective, Objective, Assessment, and Plan sections, while a Simple note will have one free-text field that will serve as the body of the note. Both SOAP and Simple notes can be labeled as a Psychotherapy note.
How to present physical examination findings?
The H/P includes considerable more detail and information versus the SOAP note which provides only that information which is relevant to addresses the problem.
What is included in an H&P?
If incorporating examination findings into a presentation, positive and relevant negative findings should be provided rather than recounting the whole examination. Providing the NEWS score and stating which observations are abnormal is good practice. This is especially important for sick patients.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Record of Physical Examination?
The Record of Physical Examination is a document that provides a detailed account of an individual's health status following a physical examination by a qualified healthcare professional.
Who is required to file Record of Physical Examination?
Typically, individuals who are applying for certain jobs, licenses, or permits may be required to file a Record of Physical Examination to demonstrate their health fitness.
How to fill out Record of Physical Examination?
To fill out the Record of Physical Examination, an individual must provide personal details, the purpose of the examination, and have a healthcare professional complete the medical evaluation and findings sections.
What is the purpose of Record of Physical Examination?
The purpose of the Record of Physical Examination is to assess an individual's health status, identify any medical conditions, and determine fitness for specific roles or activities.
What information must be reported on Record of Physical Examination?
The information that must be reported includes the individual's personal information, the date of the examination, results of the physical exam, any medical history, and recommendations from the healthcare provider.
Fill out your record of physical examination online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Record Of Physical Examination is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.