Get the free Preferred Provider Plan Reporting
Show details
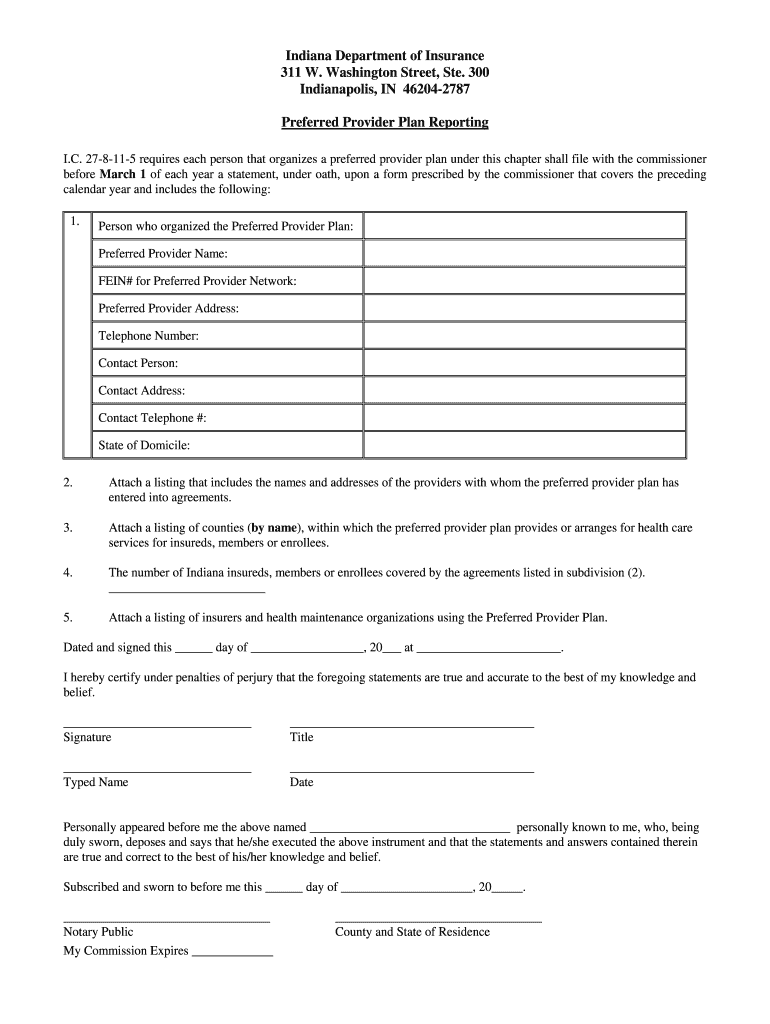
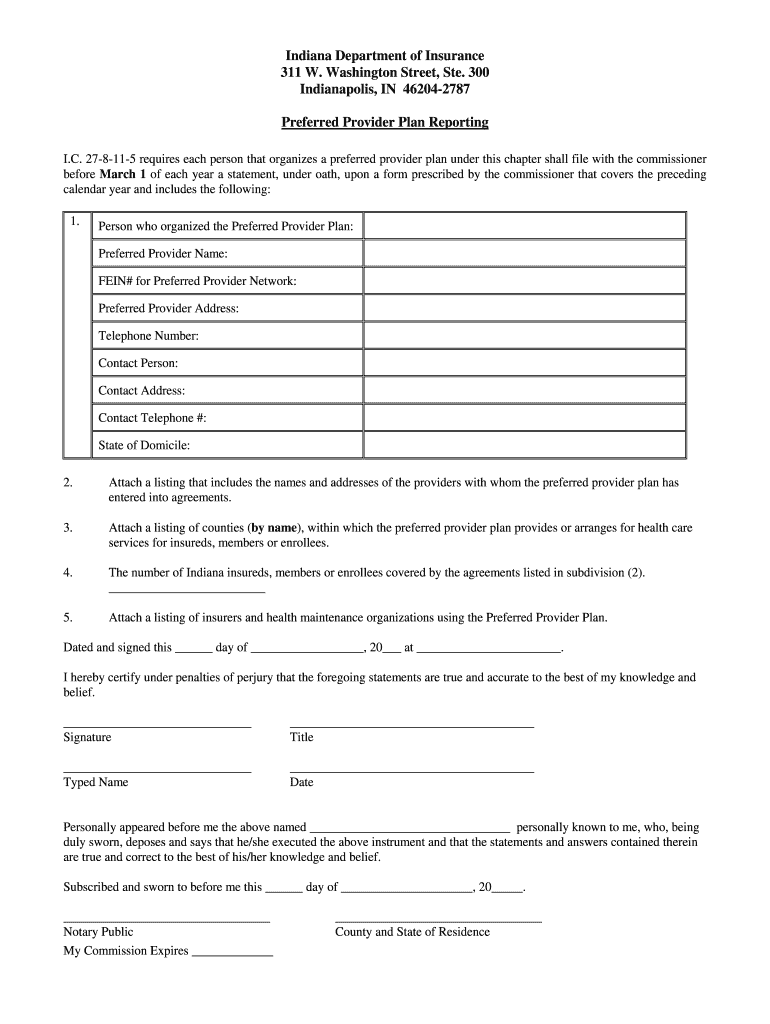
This document is required by the Indiana Department of Insurance for annual reporting by organizations that manage preferred provider plans. It includes essential information such as the organizer's
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign preferred provider plan reporting

Edit your preferred provider plan reporting form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your preferred provider plan reporting form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit preferred provider plan reporting online
Follow the steps down below to benefit from the PDF editor's expertise:
1
Sign into your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit preferred provider plan reporting. Text may be added and replaced, new objects can be included, pages can be rearranged, watermarks and page numbers can be added, and so on. When you're done editing, click Done and then go to the Documents tab to combine, divide, lock, or unlock the file.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out preferred provider plan reporting

How to fill out Preferred Provider Plan Reporting
01
Obtain the Preferred Provider Plan Reporting form from your organization's administrative office or website.
02
Review the instructions provided with the form to understand the reporting requirements.
03
Gather necessary data, including provider information, service codes, and patient details.
04
Begin filling out the form section by section, ensuring all required fields are completed.
05
Double-check the accuracy of the data entered to minimize errors.
06
If applicable, attach any supporting documentation requested in the form's instructions.
07
Review the completed form for compliance with reporting guidelines.
08
Submit the form to the designated department or individual within the specified deadline.
Who needs Preferred Provider Plan Reporting?
01
Health insurance providers who manage preferred provider networks.
02
Employers offering health benefits to their employees.
03
Medical providers participating in the preferred provider plans.
04
Regulatory bodies requiring compliance with healthcare reporting standards.
Fill
form
: Try Risk Free






People Also Ask about
What is the advantage of having a Preferred Provider Organization insurance plan?
What is “preferred provider” versus “non-preferred provider”? A preferred provider (also known as in-network provider or participating provider) has entered into an agreement with Blue Shield of California to accept our allowed amount as payment in full. This gives you the highest level of benefits.
What is the downside to a PPO plan?
Cons of PPO Plans Less Coordination: Without a primary care doctor managing your healthcare, there's less oversight, and it can be harder to keep track of your treatments and appointments. More Complex Management: Managing a PPO plan can be tricky.
What is the difference between a PPO and a PPS?
With PPO insurance, you'll pay less out of pocket when you get care within that network. You can still see an out-of-network provider, but you'll get the most coverage when you stay within the PPO network. PPO health plans may be a good fit for someone who lives in 2 different states or travels often within the U.S.
What is the difference between a preferred provider and a non-preferred provider?
1 Healthcare facilities and practitioners, known as preferred providers, offer services to the insurer's plan policyholders at reduced rates. Plan participants receive the maximum PPO benefit when they visit in-network healthcare professionals and are also offered coverage when they see out-of-network providers.
What are the two types of PPOs?
There are two types of Medicare PPO plan: Regional PPOs, which serve a single state or multi-state areas determined by Medicare. Local PPOs, which serve a single county or group of counties chosen by the plan and approved by Medicare.
What is a preferred provider plan?
Preferred provider organization (PPO) A type of medical plan in which coverage is provided to participants through a network of selected health care providers, such as hospitals and physicians. Enrollees may seek care outside the network but pay a greater percentage of the cost of coverage than within the network.
How do you use preferred provider in a sentence?
The preferred provider organization (PPO) covers a portion of the costs if Steven chooses to see a specialist outside the network. Sarah's health insurance is a preferred provider organization (PPO), allowing her flexibility in choosing her care providers.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Preferred Provider Plan Reporting?
Preferred Provider Plan Reporting is a system used to collect and report data related to health care services provided by a network of preferred providers. It helps in tracking the performance, costs, and quality of care within a preferred provider organization.
Who is required to file Preferred Provider Plan Reporting?
Health insurance plans that operate under preferred provider arrangements are required to file Preferred Provider Plan Reporting. This typically includes managed care organizations and insurers that offer network-based health plans.
How to fill out Preferred Provider Plan Reporting?
To fill out Preferred Provider Plan Reporting, organizations must gather relevant data about services provided, including patient demographics, provider details, and financial transactions. The information is then input into the designated reporting format, often using online portals or software tools provided by regulatory bodies.
What is the purpose of Preferred Provider Plan Reporting?
The purpose of Preferred Provider Plan Reporting is to enhance transparency in health care costs, evaluate provider performance, ensure compliance with regulations, and ultimately improve health care quality for consumers.
What information must be reported on Preferred Provider Plan Reporting?
Information that must be reported includes provider names, services rendered, costs of care, patient outcomes, demographic information, and any other data required by the regulatory authority overseeing the reporting process.
Fill out your preferred provider plan reporting online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Preferred Provider Plan Reporting is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















