Get the free Invitation to Negotiate Pharmacy Benefits Plan Management Services
Show details
This document serves as an invitation for negotiations regarding the management services for the Pharmacy Benefits Plan for the State of Florida, including clarification of contract terms, performance
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign invitation to negotiate pharmacy
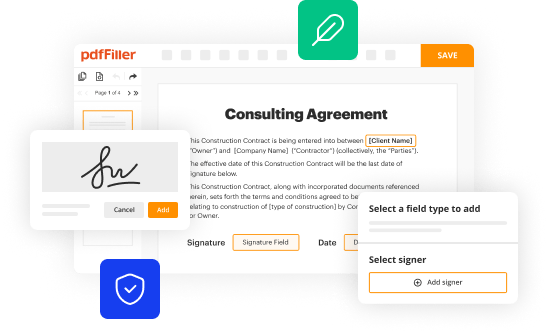
Edit your invitation to negotiate pharmacy form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
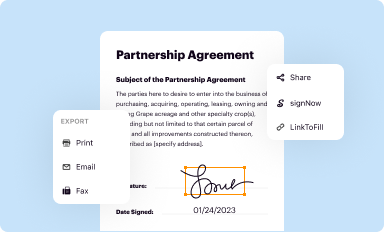
Share your form instantly
Email, fax, or share your invitation to negotiate pharmacy form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit invitation to negotiate pharmacy online
To use the professional PDF editor, follow these steps below:
1
Log into your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit invitation to negotiate pharmacy. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
With pdfFiller, it's always easy to work with documents. Try it out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out invitation to negotiate pharmacy
How to fill out Invitation to Negotiate Pharmacy Benefits Plan Management Services
01
Begin by gathering necessary information about your organization and the specific services required.
02
Create a clear and concise title for the invitation that reflects the purpose, such as 'Invitation to Negotiate Pharmacy Benefits Plan Management Services.'
03
Include an introduction that outlines the goals of the negotiation and the expected outcomes.
04
Specify the eligibility criteria for vendors who wish to respond, ensuring they meet necessary qualifications.
05
Detail the scope of work, including specific services needed, timelines, and performance expectations.
06
Outline the criteria for evaluating vendor proposals, such as pricing, experience, and service offerings.
07
Provide a deadline for submission of proposals, and outline the process for vendors to submit their responses.
08
Include any additional documentation or forms that vendors must complete as part of their proposal submission.
09
Offer contact information for questions and clarifications regarding the invitation.
10
Review and proofread the document before distribution to ensure clarity and completeness.
Who needs Invitation to Negotiate Pharmacy Benefits Plan Management Services?
01
Healthcare organizations looking to optimize their pharmacy benefits management.
02
Insurance companies that want to negotiate pharmacy services for their clients.
03
Employers seeking to manage and reduce prescription drug costs for their employees.
04
Pharmacy benefit managers (PBMs) interested in submitting proposals for managing pharmacy services.
Fill
form
: Try Risk Free






People Also Ask about
Who are the top 3 pharmacy benefit managers?
For 2025, the three largest pharmacy benefit managers (PBMs) — Caremark (CVS Health), Express Scripts (Cigna), and Optum Rx (United Health Group) — have again each excluded hundreds of drugs from their standard formularies.
Who are the big 3 pharmacy benefit managers?
The "Big 3" pharmacy benefit managers – CVS Caremark, Express Scripts and OptumRx – mark up specialty drugs at their affiliated pharmacies by hundreds or even thousands of percent, ing to a new interim staff report from the Federal Trade Commission.
How do pharmacy benefit managers make money?
PBMs also derive revenue in other ways: for example, they receive a share of the drug rebates they negotiate with pharmaceutical companies; they collect the difference between what insurers are reimbursed and the amount that pharmacies are paid (the “spread”); and they steer business to their affiliated pharmacies.
How do PBMs negotiate with pharmacies?
PBMs negotiate drug prices with manufacturers, usually by offering a spot for a drug on the payer's formulary in exchange for paying the manufacturer a lower price and receiving a rebate. PBMs may also negotiate with pharmacies, offering them a place in the payer's network for specific drug prices.
Who is the big 3 pharmacy benefit manager?
Today, there are 66 PBM companies, with the three largest – Express Scripts, CVS Caremark, and OptumRx, processing approximately 79% of all prescription drugs in 2022 and serving about 290 million Americans. PBMs are powerful but often behind-the-scenes players in the U.S. health care system.
What is pharmacy benefit management services?
What are PBMs. Pharmacy benefit managers, or PBMs, manage prescription drug benefits for clients ranging from health insurers and Medicare Part D drug plans to large employers. PBMs are one of the few parts of the prescription drug supply chain specifically dedicated to lowering costs.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Invitation to Negotiate Pharmacy Benefits Plan Management Services?
An Invitation to Negotiate Pharmacy Benefits Plan Management Services is a procurement document issued by an organization to solicit proposals from vendors for the management of pharmacy benefits. It outlines the specific services required and invites potential providers to submit their best proposals for consideration.
Who is required to file Invitation to Negotiate Pharmacy Benefits Plan Management Services?
Typically, organizations such as health plans, employers, or governmental agencies that seek to contract out pharmacy benefits management services are required to file an Invitation to Negotiate.
How to fill out Invitation to Negotiate Pharmacy Benefits Plan Management Services?
To fill out an Invitation to Negotiate, the organization must provide detailed information about the pharmacy benefits required, including service specifications, evaluation criteria, and submission guidelines for bidders. The document should also outline timelines, terms, and conditions relevant to the negotiation process.
What is the purpose of Invitation to Negotiate Pharmacy Benefits Plan Management Services?
The purpose of the Invitation to Negotiate is to enhance transparency in the procurement process, obtain competitive bids from qualified vendors, and ultimately select the best vendor to manage pharmacy benefits effectively and efficiently.
What information must be reported on Invitation to Negotiate Pharmacy Benefits Plan Management Services?
The information that must be reported includes the scope of pharmacy benefits services required, vendor qualifications, financial proposals, relevant experience and references, service delivery timelines, and compliance with regulatory requirements.
Fill out your invitation to negotiate pharmacy online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Invitation To Negotiate Pharmacy is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.