
Get the free CDPH PRE-EXISTING CONDITION INSURANCE PLAN PROGRAM APPLICATION - cdph ca
Show details
This document is an application form designed to determine eligibility for health insurance assistance under the California Department of Public Health's program for individuals with pre-existing
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign cdph pre-existing condition insurance
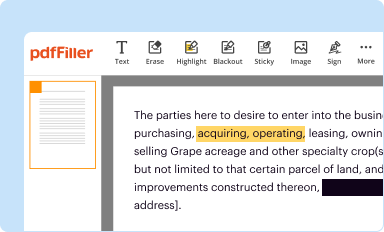
Edit your cdph pre-existing condition insurance form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
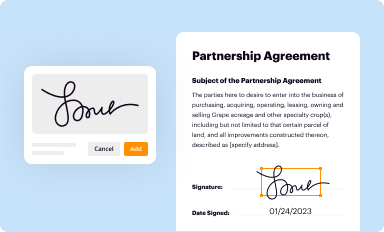
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your cdph pre-existing condition insurance form via URL. You can also download, print, or export forms to your preferred cloud storage service.
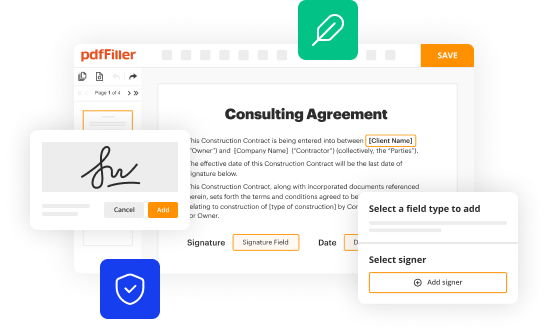
Editing cdph pre-existing condition insurance online
Follow the guidelines below to take advantage of the professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit cdph pre-existing condition insurance. Replace text, adding objects, rearranging pages, and more. Then select the Documents tab to combine, divide, lock or unlock the file.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
With pdfFiller, it's always easy to work with documents. Check it out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out cdph pre-existing condition insurance
How to fill out CDPH PRE-EXISTING CONDITION INSURANCE PLAN PROGRAM APPLICATION
01
Obtain the CDPH Pre-Existing Condition Insurance Plan Program Application from the official website or local health department.
02
Read the instructions carefully to ensure you understand the requirements.
03
Fill out the personal information section, including your name, address, and contact details.
04
Provide details about your pre-existing condition, including the diagnosis and the date of diagnosis.
05
Complete the insurance history section, indicating any existing health insurance coverage you may have.
06
Attach necessary documentation that supports your application, such as medical records or proof of previous coverage.
07
Review the application to check for accuracy and completeness.
08
Sign and date the application to certify the information provided is true to the best of your knowledge.
09
Submit the application via the specified method (mail, online, or in-person) as outlined in the instructions.
Who needs CDPH PRE-EXISTING CONDITION INSURANCE PLAN PROGRAM APPLICATION?
01
Individuals who have been denied health insurance due to a pre-existing condition.
02
People looking for affordable health insurance options specifically related to pre-existing conditions.
03
Residents of the state who meet the eligibility criteria set forth by the CDPH program.
04
Those who require immediate health coverage because of ongoing medical needs.
Fill
form
: Try Risk Free






People Also Ask about
What is the waiting period for pre-existing conditions?
Pre-existing medical conditions: A three-month wait may apply to certain prescribed minimum benefits. These constraints apply only to the pre-existing condition, and all other valid claims will be accepted, subject to the standard three-month exclusion clause if this waiting period for medical aid should still apply.
What is the maximum time period that pre-existing conditions can be excluded?
A pre-existing condition exclusion can not be longer than 12 months from your enrollment date (18 months for a late enrollee). A pre-existing condition exclusion that is applied to you must be reduced by the prior creditable coverage you have that was not interrupted by a significant break in coverage.
Do healthcare gov plans cover pre-existing conditions?
Coverage for pre-existing conditions Once you're enrolled, the plan can't deny you coverage or raise your rates based only on your health. Medicaid and the Children's Health Insurance Program (CHIP) also can't refuse to cover you or charge you more because of your pre-existing condition.
What is the pre-existing condition exclusion period?
A pre-existing condition exclusion period limits the number of benefits that an insurer has to provide for specific medical conditions and does not apply to medical benefits afforded by a health insurance policy for other types of care.
How long is a pre-existing medical condition?
The insurer will only tell you if you're covered at the time you make a claim. They won't cover you for any conditions you've had in the five years before you took out the insurance. But if you've not had treatment, medication or advice for those conditions for two years, they may cover you for them in the future.
Can I get cover for pre-existing conditions?
The insurer will only tell you if you're covered at the time you make a claim. They won't cover you for any conditions you've had in the five years before you took out the insurance. But if you've not had treatment, medication or advice for those conditions for two years, they may cover you for them in the future.
How long can a pre-existing condition be excluded in a health policy in California?
If you are joining a fully insured group health plan in California, the maximum exclusion period is 6 months. If you are joining a self-insured group health plan, the maximum exclusion period is 12 months. You will receive credit toward your pre-existing condition exclusion period for any previous continuous coverage.
What is the medicare rule for preexisting conditions?
Medicare coverage for preexisting conditions Original Medicare ( Part A and Part B ) has helped cover preexisting conditions since it began in 1965. And thanks to the Affordable Care Act signed in 2014, there are no additional costs for Original Medicare coverage if you have preexisting conditions.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is CDPH PRE-EXISTING CONDITION INSURANCE PLAN PROGRAM APPLICATION?
The CDPH Pre-Existing Condition Insurance Plan Program Application is a form used to apply for health insurance coverage for individuals with pre-existing conditions, providing access to necessary medical care.
Who is required to file CDPH PRE-EXISTING CONDITION INSURANCE PLAN PROGRAM APPLICATION?
Individuals who have been denied health insurance coverage due to pre-existing conditions are required to file the application.
How to fill out CDPH PRE-EXISTING CONDITION INSURANCE PLAN PROGRAM APPLICATION?
To fill out the application, individuals must provide personal information, details about their pre-existing conditions, and any required documentation proving their eligibility.
What is the purpose of CDPH PRE-EXISTING CONDITION INSURANCE PLAN PROGRAM APPLICATION?
The purpose of the application is to help individuals with pre-existing conditions obtain affordable health insurance coverage and ensure they have access to necessary healthcare services.
What information must be reported on CDPH PRE-EXISTING CONDITION INSURANCE PLAN PROGRAM APPLICATION?
Applicants must report their personal identification details, medical history related to pre-existing conditions, and any prior insurance coverage information.
Fill out your cdph pre-existing condition insurance online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Cdph Pre-Existing Condition Insurance is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















