
Get the free Request for Utilization Review
Show details
This document provides instructions for completing the Request for Utilization Review for the Colorado Division of Workers' Compensation. It outlines the required information and documentation needed
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign request for utilization review
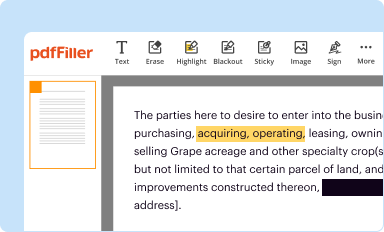
Edit your request for utilization review form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
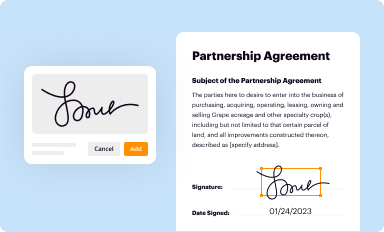
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your request for utilization review form via URL. You can also download, print, or export forms to your preferred cloud storage service.
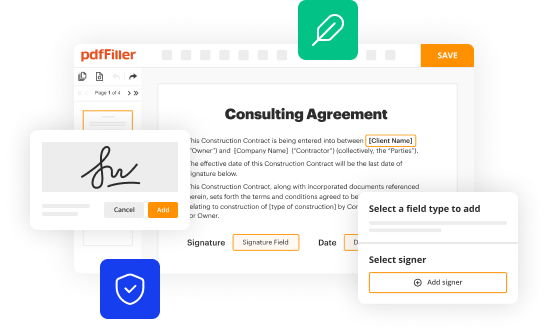
Editing request for utilization review online
In order to make advantage of the professional PDF editor, follow these steps below:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit request for utilization review. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
Dealing with documents is simple using pdfFiller.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out request for utilization review
How to fill out Request for Utilization Review
01
Start by obtaining the Request for Utilization Review form from the appropriate source.
02
Fill out the patient's information, including name, date of birth, and identification number.
03
Provide the details of the healthcare provider, including name, address, and contact information.
04
Specify the diagnosis and the treatment or service being requested for review.
05
Include any relevant medical history or previous treatments related to the request.
06
Clearly state the clinical rationale for the requested service or treatment.
07
Attach any supporting documents, such as test results or referral letters.
08
Review the completed form for accuracy and completeness.
09
Submit the form to the designated Utilization Review organization or insurance company.
Who needs Request for Utilization Review?
01
Healthcare providers who require authorization for specific medical services.
02
Patients seeking approval for treatments that may not be covered under their insurance plans.
03
Insurance companies that need to evaluate the medical necessity of proposed treatments.
04
Facilities providing care, such as hospitals or clinics, that require validation of services rendered.
Fill
form
: Try Risk Free






People Also Ask about
What is the utilization review process?
Utilization reviews serve to evaluate each patient's care before, during and after procedures to ensure they receive adequate care throughout their hospital stay. Some UR nurses may oversee patient discharge and play a role in designing after-care plans, referred to as case management.
What is an ur?
Utilization review can be done by a peer review group, or a public agency. UR is a method of tracking, reviewing and rendering opinions regarding care provided to patients. Usually UR involves the use of protocols, benchmarks or data with which to compare specific cases to an aggregate set of cases.
What are the steps in the utilization review process?
Reviews happen in these three stages: Prospective: In this stage, a patient seeks approval in preparation for care. Concurrent: Reviews take place during care to evaluate medical necessity. Retrospective: This review evaluates after-care plans including outpatient therapies.
What are the basic three components of utilization review?
There are three activities within the utilization review process: prospective, concurrent and retrospective.
What is the difference between CDI and utilization review?
The goal of CDI specialists is to ensure that documentation accurately reflects the patient's condition and care provided, a process that is essential to avoid denials and ensure proper reimbursement. Utilization management involves evaluating the appropriateness and medical necessity of care services.
How do you use utilization review in a sentence?
Systematic utilization review coupled with assessment of patients' needs and preferences should be incorporated into the priority-setting process to balance the emphasis on new technologies.
What is the drug utilization review process?
Drug utilization review refers to a review of prescribing, dispensing, administering and ingesting of medication. This authorized, structured and ongoing review is related to pharmacy benefit managers. Drug use/ utilization evaluation and medication utilization evaluations are the same as drug utilization review.
What is the purpose of the insurance claim utilization review process?
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Request for Utilization Review?
A Request for Utilization Review is a formal process used by healthcare providers to seek authorization for medical services or procedures to ensure they are medically necessary and covered by insurance.
Who is required to file Request for Utilization Review?
Typically, healthcare providers, such as doctors or hospitals, are required to file a Request for Utilization Review on behalf of patients when seeking approval for certain treatments or services.
How to fill out Request for Utilization Review?
To fill out a Request for Utilization Review, you need to provide patient information, details of the proposed treatment or service, supporting medical documentation, and the justification for the request.
What is the purpose of Request for Utilization Review?
The purpose of a Request for Utilization Review is to evaluate the medical necessity and appropriateness of proposed healthcare services before they are provided to ensure compliance with insurance coverage policies.
What information must be reported on Request for Utilization Review?
Information that must be reported includes patient demographics, details of the requested service, clinical information supporting the necessity of the treatment, and any prior treatments or evaluations related to the request.
Fill out your request for utilization review online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Request For Utilization Review is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















