Get the free Coordination of Benefits / Direct Claim Form - state il
Show details
Este formulario se utiliza para enviar reclamos bajo las reglas de Coordinación de Beneficios. Debe completar un formulario de reclamo separado para cada farmacia utilizada y para cada paciente.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign coordination of benefits direct
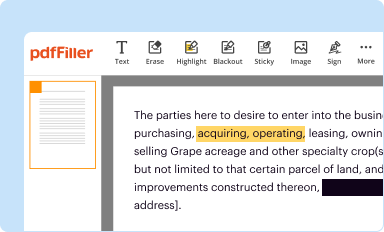
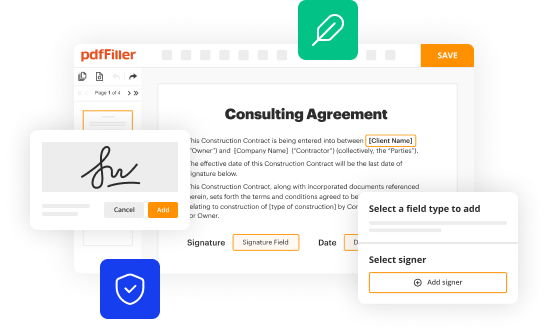
Edit your coordination of benefits direct form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
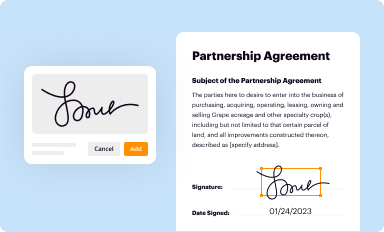
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
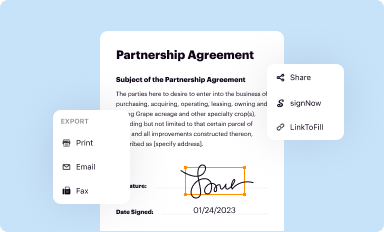
Share your form instantly
Email, fax, or share your coordination of benefits direct form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing coordination of benefits direct online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit coordination of benefits direct. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
With pdfFiller, it's always easy to deal with documents.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out coordination of benefits direct
How to fill out Coordination of Benefits / Direct Claim Form
01
Gather the necessary documents including your insurance cards and any related medical bills.
02
Identify the primary and secondary insurance policies.
03
Start filling out your personal information including your name, address, and policy numbers.
04
Provide detailed information about the medical services received, including the date of service and provider details.
05
Indicate the primary insurer and enter their information accordingly.
06
Document any payments made by the primary insurance.
07
Fill out the secondary insurance information, if applicable.
08
Review all entries for accuracy before submitting the form.
09
Sign and date the form where required.
10
Submit the form along with any supporting documents to the appropriate insurance company.
Who needs Coordination of Benefits / Direct Claim Form?
01
Individuals who have multiple health insurance policies.
02
Patients seeking reimbursement for medical services from their secondary insurance.
03
Healthcare providers filing claims for patients with coverage from more than one insurer.
04
Anyone who requires coordination between their primary and secondary insurance to avoid coverage disputes.
Fill
form
: Try Risk Free






People Also Ask about
How do you complete the coordination of benefits?
To set up coordination of benefits, you will need to contact your insurance company. Your insurance company will ask you to fill out a form disclosing any other health plans you may have in place. To gather this information your insurance company may: send you a form in the mail.
What is the problem with coordination of benefits?
Coordination of benefits (COB) errors can be a major pain point for providers, leading to costly denials and significant delays in payment. When multiple insurance plans are involved, determining which insurer is responsible for payment first is crucial.
What is a coordination of benefits form?
For example, suppose you visit your doctor and get billed $250 for the appointment. Your primary health plan may cover the majority of the bill. Let's say, for example, that's $200. Then your secondary plan would pay the remaining $50.
What is a denial for coordination of benefits?
Coordination of Benefits (COB): This denial code indicates that the patient has another insurance plan that should be billed first before the current claim. It could be that the patient has multiple insurance policies, such as primary and secondary coverage, and the primary insurer needs to be billed first.
Can a claim be denied for coordination of benefits?
Claim Denials: Incorrect coordination of benefits can lead to claim denials or overpayments. This not only affects revenue but also strains the patient-provider relationship when patients are billed incorrectly.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Coordination of Benefits / Direct Claim Form?
The Coordination of Benefits / Direct Claim Form is a document used to determine the order of payment when an individual has multiple health insurance plans. It facilitates the process of claiming benefits from various insurers to ensure that the patient is not overpaid or underpaid for their medical expenses.
Who is required to file Coordination of Benefits / Direct Claim Form?
Individuals who are covered by more than one health insurance policy are required to file the Coordination of Benefits / Direct Claim Form. This applies to dependents who may have coverage through both parents' plans as well.
How to fill out Coordination of Benefits / Direct Claim Form?
To fill out the Coordination of Benefits / Direct Claim Form, a person must provide personal information, details about both insurance policies, the nature of the medical services received, and the costs associated with those services. Accurate information about the primary and secondary insurers is essential.
What is the purpose of Coordination of Benefits / Direct Claim Form?
The purpose of the Coordination of Benefits / Direct Claim Form is to establish which insurance policy is primary and which is secondary when processing claims. This ensures that healthcare providers are reimbursed correctly and prevents conflict over payments between insurers.
What information must be reported on Coordination of Benefits / Direct Claim Form?
The information that must be reported on the Coordination of Benefits / Direct Claim Form includes the policyholder's personal details, insurance company information for both primary and secondary coverage, details of the medical service provided, associated costs, and any other relevant claim information.
Fill out your coordination of benefits direct online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Coordination Of Benefits Direct is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.