
Get the free Utilization management program - Mercy Provider Network - mercyoptions
Show details
Resolution offers 3 methods to request authorizations. Choose the most convenient method for you. Web Portal www.medsolutionsonline.com Resolutions is available online 24/7. After a quick and easy
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign utilization management program
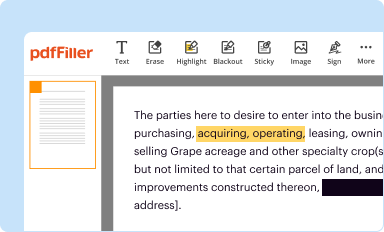
Edit your utilization management program form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
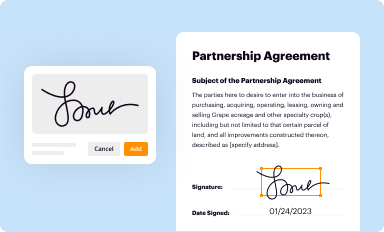
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
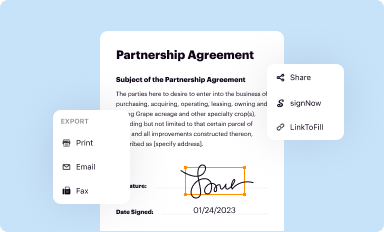
Share your form instantly
Email, fax, or share your utilization management program form via URL. You can also download, print, or export forms to your preferred cloud storage service.
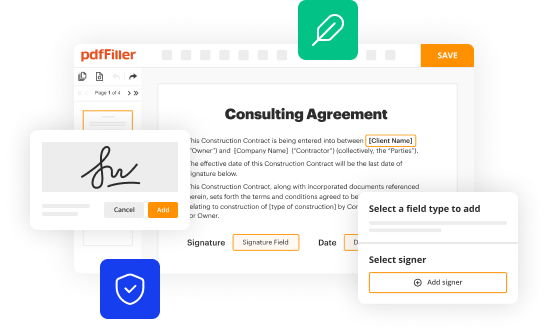
Editing utilization management program online
To use the services of a skilled PDF editor, follow these steps:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit utilization management program. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out utilization management program
How to fill out utilization management program:
01
Understand the purpose: Before you start filling out the utilization management program, it is crucial to have a clear understanding of its purpose. This program is designed to ensure that the utilization of resources, services, or treatments within an organization is appropriate, efficient, and cost-effective. Familiarize yourself with any guidelines, regulations, or requirements related to this program.
02
Gather necessary information: Begin by collecting all the relevant information needed to fill out the utilization management program. This may include details about the organization, such as its goals, mission, and objectives. Additionally, you will need information about the specific resources, services, or treatments that will be managed through this program.
03
Define utilization criteria: One of the key components of a utilization management program is establishing clear utilization criteria. Determine the standards or benchmarks against which the utilization of resources, services, or treatments will be evaluated. These criteria should be based on evidence, best practices, industry standards, and the specific needs of your organization.
04
Develop utilization review processes: Outline the processes and procedures that will be used to review and assess the utilization of resources, services, or treatments. This may include developing review forms, creating workflows, and establishing decision-making protocols. Ensure that these processes are clear, well-documented, and easily understandable by those involved.
05
Involve the relevant stakeholders: It is essential to involve all the relevant stakeholders in the utilization management program. This may include healthcare providers, administrators, managers, and other personnel involved in the decision-making processes. Collaborate with these stakeholders to gather their input, address their concerns, and ensure their buy-in for the program.
06
Implement and monitor the program: Once the utilization management program has been filled out, it is time to implement it. This may involve training staff, educating stakeholders, and integrating the program into the organization's existing processes. Continuously monitor the program's effectiveness, gather data, and make necessary adjustments to improve its outcomes.
Who needs utilization management program:
01
Healthcare organizations: Utilization management programs are particularly crucial for healthcare organizations, such as hospitals, clinics, and insurance companies. These entities need to ensure that the utilization of healthcare resources, services, or treatments is appropriate and cost-effective.
02
Insurance providers: Insurance providers often implement utilization management programs to control costs and ensure that the services or treatments covered by their policies are necessary and used appropriately. This helps prevent unnecessary or redundant utilization of resources, ultimately reducing expenses.
03
Employers: Many employers offer healthcare benefits to their employees, and utilizing utilization management programs can help them ensure that these benefits are used efficiently. By managing the utilization of healthcare services, employers can control expenses and optimize the value of the benefits they provide.
04
Government agencies: Government agencies responsible for healthcare regulation and oversight may implement utilization management programs to ensure the appropriate use of resources in the public healthcare system. This helps in controlling costs, improving patient outcomes, and ensuring equitable access to healthcare services.
05
Healthcare professionals: Healthcare professionals, including physicians, nurses, and other providers, can also benefit from utilization management programs. These programs provide them with guidelines and criteria for making informed decisions about the utilization of resources, services, or treatments, ultimately improving patient care.
In conclusion, filling out a utilization management program requires understanding its purpose, gathering necessary information, defining utilization criteria, developing review processes, involving stakeholders, and continuously monitoring the program. This program is needed by healthcare organizations, insurance providers, employers, government agencies, and healthcare professionals to ensure appropriate and cost-effective utilization of resources, services, or treatments.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit utilization management program in Chrome?
Add pdfFiller Google Chrome Extension to your web browser to start editing utilization management program and other documents directly from a Google search page. The service allows you to make changes in your documents when viewing them in Chrome. Create fillable documents and edit existing PDFs from any internet-connected device with pdfFiller.
How can I fill out utilization management program on an iOS device?
In order to fill out documents on your iOS device, install the pdfFiller app. Create an account or log in to an existing one if you have a subscription to the service. Once the registration process is complete, upload your utilization management program. You now can take advantage of pdfFiller's advanced functionalities: adding fillable fields and eSigning documents, and accessing them from any device, wherever you are.
How do I edit utilization management program on an Android device?
With the pdfFiller mobile app for Android, you may make modifications to PDF files such as utilization management program. Documents may be edited, signed, and sent directly from your mobile device. Install the app and you'll be able to manage your documents from anywhere.
What is utilization management program?
Utilization management program is a process used by insurance companies to review and manage the use of healthcare services to ensure they are medically necessary and cost-effective.
Who is required to file utilization management program?
Insurance companies and healthcare providers are required to file utilization management programs.
How to fill out utilization management program?
Utilization management programs can be filled out by detailing the procedures and criteria used to determine the medical necessity and appropriateness of healthcare services.
What is the purpose of utilization management program?
The purpose of utilization management programs is to ensure that healthcare services are utilized effectively and efficiently, while maintaining quality of care.
What information must be reported on utilization management program?
Utilization management programs must include information on the criteria used to make utilization review decisions, the types of services reviewed, and the outcomes of the reviews.
Fill out your utilization management program online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Utilization Management Program is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















