Get the free PROVIDER NETWORK ADEQUACY
Show details
PROVIDER NETWORK ADEQUACY
INSTRUCTIONSMANAGED CARE SYSTEMSPROVIDER NETWORK ADEQUACY INSTRUCTIONS Minnesota Department of Health
Managed Care Systems
PO Box 64882,
St. Paul, MN 551640882
6512015100
health.managedcare@state.mn.us
www.health.state.mn.usUpon
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign provider network adequacy
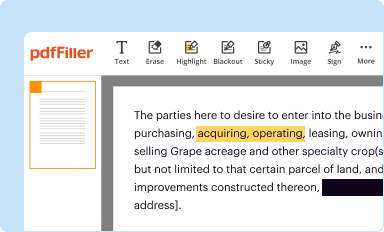
Edit your provider network adequacy form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
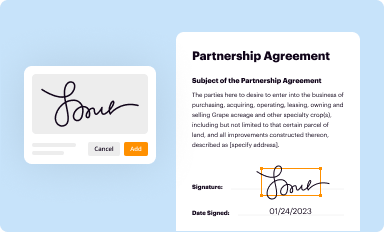
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
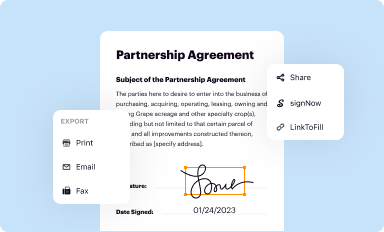
Share your form instantly
Email, fax, or share your provider network adequacy form via URL. You can also download, print, or export forms to your preferred cloud storage service.
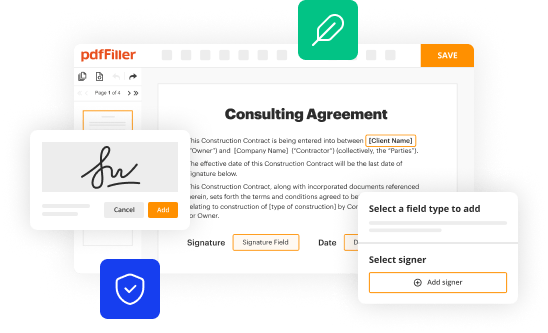
Editing provider network adequacy online
To use our professional PDF editor, follow these steps:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit provider network adequacy. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out provider network adequacy
How to fill out provider network adequacy:
01
Research the requirements: The first step in filling out provider network adequacy is to carefully review the guidelines and requirements set by the relevant regulatory body or insurance provider. Understand what qualifies as a "provider network" and what criteria need to be met for adequacy.
02
Assess the current network: Evaluate your existing network of healthcare providers and determine if it meets the required standards. Consider factors such as geographical coverage, specialty availability, and the number of providers within each specialty.
03
Identify any gaps: Identify any gaps or deficiencies in your provider network. This may involve analyzing areas with limited provider access or identifying specialties that are underrepresented. Highlight these gaps for further action.
04
Develop a recruitment plan: If your network is lacking in certain areas, develop a plan to recruit additional providers. This may involve reaching out to healthcare professionals, posting job openings, or collaborating with medical organizations to attract providers in the needed specialties or areas.
05
Conduct provider outreach: Reach out to potential providers and establish a dialogue. Provide them with information about your network and inquire about their interest in joining. Gauge their willingness to participate and assess if they meet the necessary qualifications.
06
Evaluate participation agreements: Review your existing provider participation agreements or contracts. Ensure they include provisions that align with the network adequacy requirements. Update or modify contracts as needed to comply with the regulatory guidelines.
07
Document efforts: Keep thorough documentation of your recruitment efforts, including communication with providers, outreach activities, and any changes made to contracts. This documentation will be important if audited or if you need to demonstrate compliance.
Who needs provider network adequacy:
01
Insurance providers: Insurance companies must ensure that their provider networks adequately meet the needs of their policyholders. This includes offering a sufficient number of providers covering various specialties and geographical areas.
02
Regulatory bodies: Government agencies or regulatory bodies responsible for overseeing healthcare insurance may require insurance providers to demonstrate network adequacy. This is done to protect consumers and ensure they have access to necessary medical services.
03
Healthcare organizations: Healthcare organizations that contract with insurers to provide services to their patients also need to consider provider network adequacy. They must ensure that the network offered by the insurance company aligns with the needs of their patients and meets the standards set by regulatory bodies.
In summary, filling out provider network adequacy involves researching requirements, assessing the current network, identifying gaps, developing a recruitment plan, conducting provider outreach, evaluating participation agreements, and documenting efforts. Insurance providers, regulatory bodies, and healthcare organizations all have an interest in ensuring network adequacy.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get provider network adequacy?
The pdfFiller premium subscription gives you access to a large library of fillable forms (over 25 million fillable templates) that you can download, fill out, print, and sign. In the library, you'll have no problem discovering state-specific provider network adequacy and other forms. Find the template you want and tweak it with powerful editing tools.
How do I fill out provider network adequacy using my mobile device?
On your mobile device, use the pdfFiller mobile app to complete and sign provider network adequacy. Visit our website (https://edit-pdf-ios-android.pdffiller.com/) to discover more about our mobile applications, the features you'll have access to, and how to get started.
How do I fill out provider network adequacy on an Android device?
Use the pdfFiller app for Android to finish your provider network adequacy. The application lets you do all the things you need to do with documents, like add, edit, and remove text, sign, annotate, and more. There is nothing else you need except your smartphone and an internet connection to do this.
What is provider network adequacy?
Provider network adequacy refers to the requirement for insurance providers to maintain an adequate network of healthcare providers to ensure that their members have access to necessary medical services.
Who is required to file provider network adequacy?
Insurance providers are required to file provider network adequacy to demonstrate compliance with state regulations.
How to fill out provider network adequacy?
Insurance providers can fill out provider network adequacy forms by providing information about the number and types of healthcare providers in their network, as well as data on member satisfaction and access to care.
What is the purpose of provider network adequacy?
The purpose of provider network adequacy is to ensure that insurance plan members have access to a sufficient number and variety of healthcare providers to meet their medical needs.
What information must be reported on provider network adequacy?
Information that must be reported on provider network adequacy includes the number and types of healthcare providers in the network, geographic distribution of providers, member access to care, and any network deficiencies.
Fill out your provider network adequacy online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Provider Network Adequacy is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.