Get the free empirx health prior authorization form
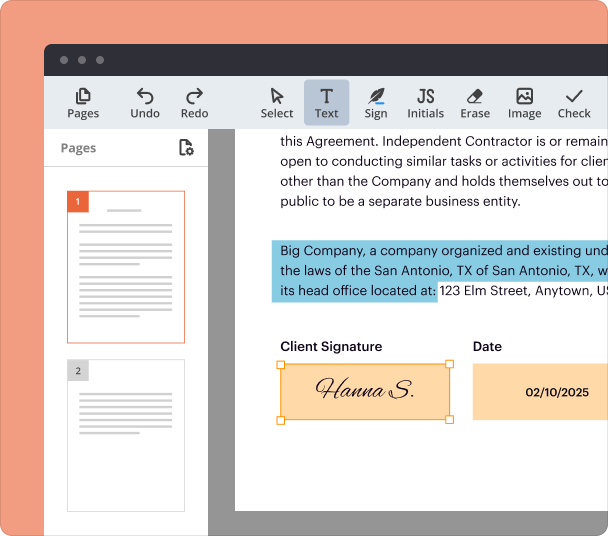
Fill out, sign, and share forms from a single PDF platform
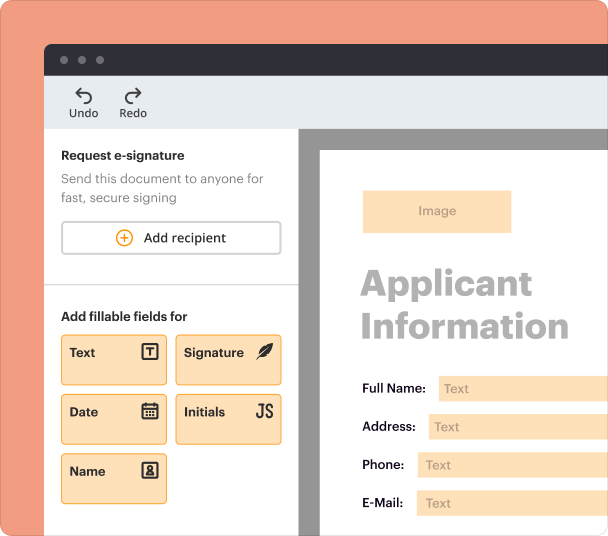
Edit and sign in one place
Create professional forms
Simplify data collection
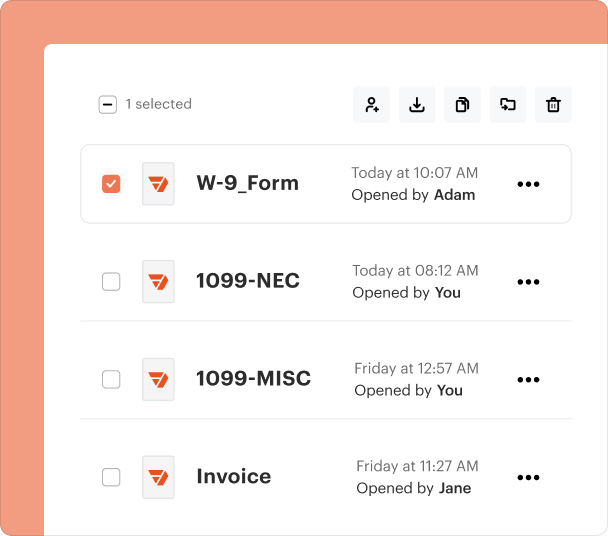
Manage forms centrally
Why pdfFiller is the best tool for your documents and forms
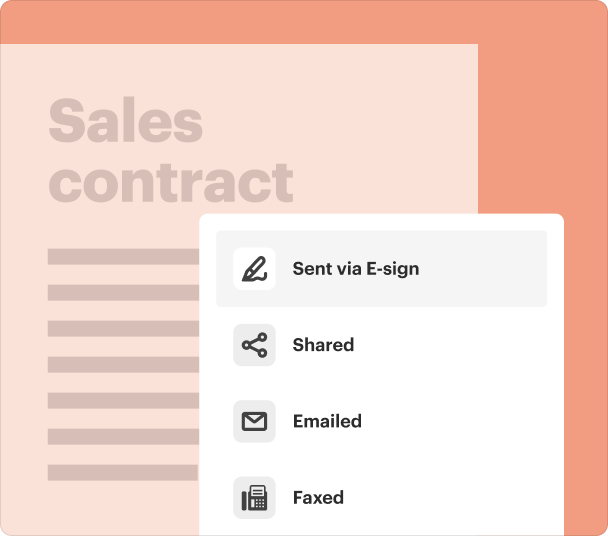
End-to-end document management
Accessible from anywhere
Secure and compliant
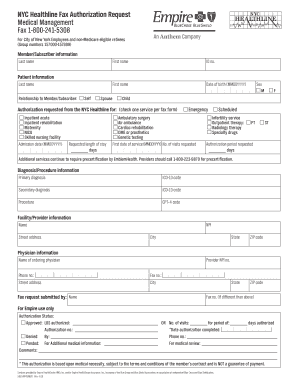
Understanding the Empirx Health Prior Authorization Form
What is the Empirx Health Prior Authorization Form?
The Empirx Health prior authorization form is a crucial document used in the healthcare system to obtain approval for certain medical services or medications required by patients. It ensures that insurance companies assess the necessity of treatments before they are administered, thereby playing a vital role in controlling healthcare costs and ensuring patients receive appropriate care.
Key Features of the Empirx Health Prior Authorization Form
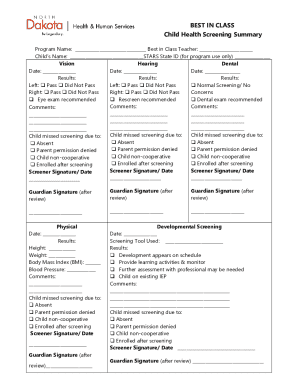
This form includes important sections for patient information, prescriber details, and clinical data. Key features might include:
-
Fields for the patient's name, contact details, and insurance information.
-
Details regarding the healthcare provider submitting the request.
-
Necessary medical information, such as diagnosis codes and lab results, relevant for the treatment.
-
Guidance on how to submit the form, either electronically or via fax.
Eligibility Criteria for the Empirx Health Prior Authorization Form
Eligibility for using the Empirx Health prior authorization form generally depends on the patient's specific insurance plan and the treatment being requested. Insurance carriers may specify conditions under which prior authorization is required, typically involving high-cost medications, specialized treatments, or specific medical conditions. It is essential for healthcare providers to verify these criteria to avoid delays in patient care.
Required Documents and Information
Completing the Empirx Health prior authorization form accurately is vital for efficient processing. Key documents and information generally required include:
-
Policy number, group number, and payer details.
-
ICD codes that justify the medical necessity of the requested treatment.
-
Details about the medication or service requested, including dosage and frequency.
-
Relevant medical history that supports the authorization request.
Common Errors and Troubleshooting
When filling out the Empirx Health prior authorization form, certain common mistakes can lead to delays or denials. Providers should check for the following issues:
-
Ensure all required fields are filled out, including patient and provider details.
-
Verify that diagnosis and procedure codes are accurate and up to date.
-
Attach all necessary clinical records and lab results to substantiate the request.
How to Fill the Empirx Health Prior Authorization Form
Filling out the Empirx Health prior authorization form requires careful attention to detail. Follow these guidelines for accurate completion:
-
Collect all patient and treatment details before starting to fill out the form.
-
Complete the form section by section, ensuring proper flow and relevance of information.
-
Carefully check the form for any errors or omissions prior to sending it off.
Frequently Asked Questions about empirx prior authorization form
What should I do if my request is denied?
If a prior authorization request is denied, review the reasons provided by the insurance company. You can often appeal the decision by submitting additional information or corrections as needed. Consulting with the prescribing physician may also be beneficial.
Can I submit the Empirx Health prior authorization form electronically?
Yes, many healthcare providers are able to submit the Empirx Health prior authorization form electronically through their practice management systems or through insurance company portals.
pdfFiller scores top ratings on review platforms