
Get the free Oral PLPrior Authorization Criteria Formdocx
Show details
Prior Authorization Criteria Form ARKANSAS BLUE CROSS BLUE SHIELD Median Rx (PDP), Median Advantage (OFFS), and Median Advantage St. Vincent (PPO) Oral Post Limit (Medicare Prior Authorization) This
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign oral plprior authorization criteria
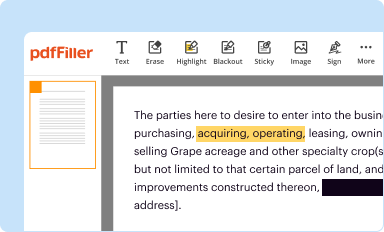
Edit your oral plprior authorization criteria form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
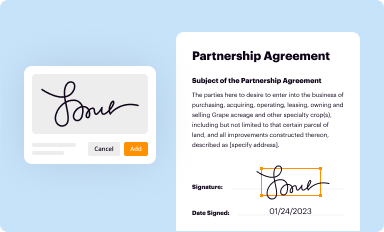
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
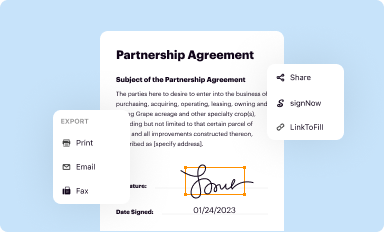
Share your form instantly
Email, fax, or share your oral plprior authorization criteria form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit oral plprior authorization criteria online
To use the services of a skilled PDF editor, follow these steps below:
1
Sign into your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
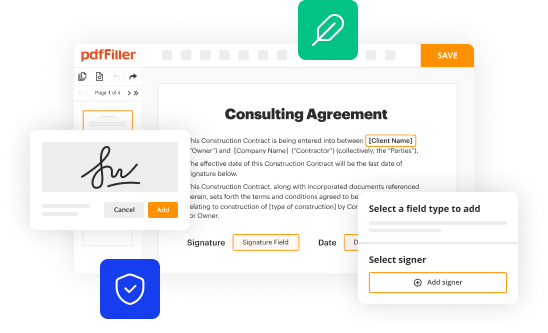
Edit oral plprior authorization criteria. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
It's easier to work with documents with pdfFiller than you can have believed. Sign up for a free account to view.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out oral plprior authorization criteria
How to fill out oral plprior authorization criteria:
01
Start by gathering all the necessary documents and information required for the authorization process. This may include patient information, medical records, prescription details, and any other relevant documentation.
02
Familiarize yourself with the specific criteria and guidelines for oral plprior authorization. Different insurance providers or healthcare organizations may have different requirements, so make sure you are using the correct criteria for your situation.
03
Carefully review the patient's medical history and condition to assess if they meet the necessary criteria for oral plprior authorization. Take note of any specific conditions or factors that need to be addressed.
04
Complete the appropriate authorization forms or documentation, ensuring that all required fields are filled out accurately and completely. Pay attention to any specific instructions or additional information that may be needed.
05
Attach all supporting documents and medical records as required. These may include test results, specialist referrals, or any other relevant information that reinforces the need for oral plprior authorization.
06
Double-check all the information provided to ensure its accuracy. Mistakes or missing information can cause delays in the authorization process.
07
Submit the completed authorization request, either electronically or through the designated channels specified by the insurance provider or healthcare organization. Keep a record of the submission for future reference.
Who needs oral plprior authorization criteria?
01
Patients who require specific medications or treatments, such as oral plprior, may need to go through the authorization process to ensure the insurance company or healthcare organization covers the cost.
02
Healthcare professionals, including doctors, specialists, and pharmacists, might need to consider and complete oral plprior authorization criteria for their patients to ensure appropriate medication access.
03
Insurance providers and healthcare organizations require oral plprior authorization criteria to evaluate the medical necessity and cost-effectiveness of the treatment before approving coverage.
04
Pharmacy benefit managers may utilize oral plprior authorization criteria to assess whether the prescribed medication aligns with their formulary or cost-management strategies.
Overall, both patients and healthcare professionals need to be aware of and follow the oral plprior authorization criteria to navigate the process effectively and ensure the necessary medications or treatments are accessible.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is oral plprior authorization criteria?
Oral plprior authorization criteria are specific requirements that need to be met before a dental procedure can be approved for coverage under a patient's insurance plan.
Who is required to file oral plprior authorization criteria?
Dental providers are usually required to file oral plprior authorization criteria with the patient's insurance company in order to request approval for a dental procedure.
How to fill out oral plprior authorization criteria?
Oral plprior authorization criteria are typically filled out by the dental provider, who will need to provide detailed information about the patient, the dental procedure, and the medical necessity of the treatment.
What is the purpose of oral plprior authorization criteria?
The purpose of oral plprior authorization criteria is to ensure that dental procedures are necessary and appropriate before they are approved for coverage, helping to control costs and prevent unnecessary or excessive treatments.
What information must be reported on oral plprior authorization criteria?
The information required on oral plprior authorization criteria may include patient demographics, procedure codes, tooth numbers, diagnostic information, treatment plans, and supporting documentation.
Where do I find oral plprior authorization criteria?
With pdfFiller, an all-in-one online tool for professional document management, it's easy to fill out documents. Over 25 million fillable forms are available on our website, and you can find the oral plprior authorization criteria in a matter of seconds. Open it right away and start making it your own with help from advanced editing tools.
Can I sign the oral plprior authorization criteria electronically in Chrome?
Yes, you can. With pdfFiller, you not only get a feature-rich PDF editor and fillable form builder but a powerful e-signature solution that you can add directly to your Chrome browser. Using our extension, you can create your legally-binding eSignature by typing, drawing, or capturing a photo of your signature using your webcam. Choose whichever method you prefer and eSign your oral plprior authorization criteria in minutes.
How can I edit oral plprior authorization criteria on a smartphone?
You can do so easily with pdfFiller’s applications for iOS and Android devices, which can be found at the Apple Store and Google Play Store, respectively. Alternatively, you can get the app on our web page: https://edit-pdf-ios-android.pdffiller.com/. Install the application, log in, and start editing oral plprior authorization criteria right away.
Fill out your oral plprior authorization criteria online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Oral Plprior Authorization Criteria is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















