
Get the free PRIOR AUTHORIZATION CRITERIA Generic
Show details
Date PRIOR AUTHORIZATION CRITERIA Generic Prescriber Last Name: Prescriber First Name: Prescriber Phone: Prescriber Fax: Patient ID# DOB **FAILURE TO COMPLETE THE FORM MAY RESULT IN A DELAY OR AN
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign prior authorization criteria generic
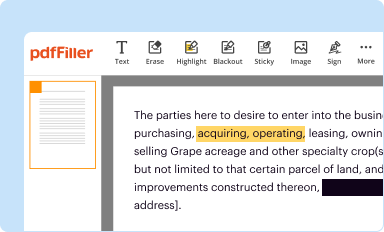
Edit your prior authorization criteria generic form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
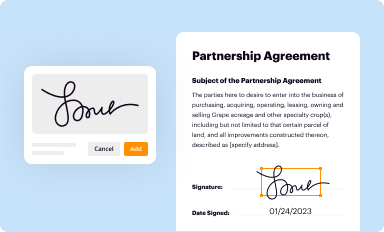
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
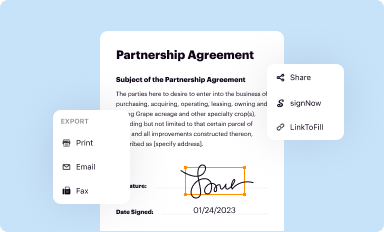
Share your form instantly
Email, fax, or share your prior authorization criteria generic form via URL. You can also download, print, or export forms to your preferred cloud storage service.
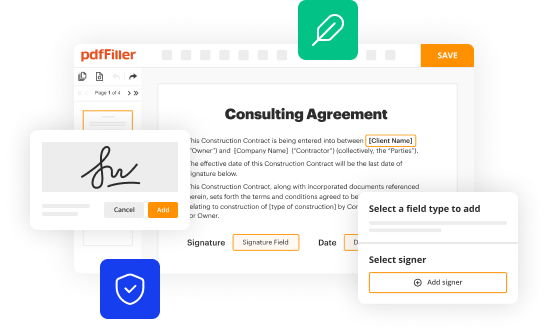
Editing prior authorization criteria generic online
In order to make advantage of the professional PDF editor, follow these steps below:
1
Check your account. In case you're new, it's time to start your free trial.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit prior authorization criteria generic. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
pdfFiller makes dealing with documents a breeze. Create an account to find out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out prior authorization criteria generic
How to fill out prior authorization criteria generic:
01
Gather all necessary information: Before filling out the prior authorization criteria for a generic medication, make sure you have all the required information handy. This includes the patient's name, date of birth, insurance information, and details about the medication being prescribed.
02
Review the specific requirements: Different insurance companies and healthcare providers may have their own sets of guidelines and criteria for prior authorization. Familiarize yourself with these requirements before starting the process to ensure that you provide all the necessary information.
03
Complete the prior authorization form: Fill out the prior authorization form accurately and completely. Make sure to provide all the relevant details about the patient and the medication being prescribed. Double-check for any errors or missing information before submitting the form.
04
Include supporting documentation: In some cases, supporting documentation may be required to justify the need for the generic medication. This can include medical records, lab results, or a letter of medical necessity from the prescribing healthcare provider. Attach these documents to the prior authorization form, if necessary.
05
Submit the prior authorization request: Once you have filled out the form and attached any required documentation, submit the prior authorization request to the appropriate party. This may be the insurance company, pharmacy benefits manager, or healthcare provider, depending on the specific process followed by your organization.
Who needs prior authorization criteria generic?
01
Patients with health insurance: Prior authorization criteria for a generic medication is required for patients who have health insurance coverage. Different insurance plans may have varying requirements, so it is essential to ensure compliance with the specific guidelines of the patient's insurance provider.
02
Healthcare providers: Healthcare providers, including doctors, nurse practitioners, and physician assistants, follow prior authorization criteria for generic medications to ensure the proper utilization of healthcare resources. This allows them to prescribe cost-effective options to their patients while adhering to the guidelines set by the insurance companies.
03
Pharmacies and pharmacy benefit managers: Pharmacies and pharmacy benefit managers play a crucial role in the prior authorization process. They review the submitted requests and ensure that the criteria for prescribing a generic medication are met before approving the prescription and providing coverage for the medication.
Note: The specific process for filling out prior authorization criteria generic may vary depending on the healthcare organization, insurance provider, and local regulations. It is recommended to consult with the respective parties involved for detailed instructions and guidance.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is prior authorization criteria generic?
Prior authorization criteria generic refers to the set of guidelines and requirements that must be met in order for a medication to be approved for coverage by an insurance provider.
Who is required to file prior authorization criteria generic?
Healthcare providers, such as physicians or pharmacists, are typically required to file prior authorization criteria generic on behalf of their patients.
How to fill out prior authorization criteria generic?
Prior authorization criteria generic can be filled out by providing the necessary medical information, documentation, and justification for why a specific medication is necessary for a patient's treatment.
What is the purpose of prior authorization criteria generic?
The purpose of prior authorization criteria generic is to ensure that medications are prescribed appropriately and that coverage is provided for medically necessary treatments.
What information must be reported on prior authorization criteria generic?
The information that must be reported on prior authorization criteria generic typically includes the patient's medical history, diagnosis, treatment plan, and the specific medication being requested for coverage.
How can I manage my prior authorization criteria generic directly from Gmail?
You may use pdfFiller's Gmail add-on to change, fill out, and eSign your prior authorization criteria generic as well as other documents directly in your inbox by using the pdfFiller add-on for Gmail. pdfFiller for Gmail may be found on the Google Workspace Marketplace. Use the time you would have spent dealing with your papers and eSignatures for more vital tasks instead.
How can I send prior authorization criteria generic to be eSigned by others?
Once you are ready to share your prior authorization criteria generic, you can easily send it to others and get the eSigned document back just as quickly. Share your PDF by email, fax, text message, or USPS mail, or notarize it online. You can do all of this without ever leaving your account.
How do I complete prior authorization criteria generic on an iOS device?
Install the pdfFiller app on your iOS device to fill out papers. If you have a subscription to the service, create an account or log in to an existing one. After completing the registration process, upload your prior authorization criteria generic. You may now use pdfFiller's advanced features, such as adding fillable fields and eSigning documents, and accessing them from any device, wherever you are.
Fill out your prior authorization criteria generic online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Prior Authorization Criteria Generic is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















