
Get the free History and Physical Form
Show details
A medical form used for gathering patient history and physical examination details in a neurosurgery context.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign history and physical form
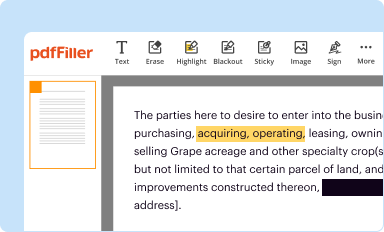
Edit your history and physical form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
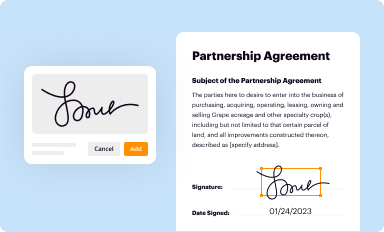
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
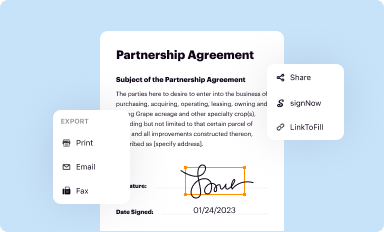
Share your form instantly
Email, fax, or share your history and physical form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
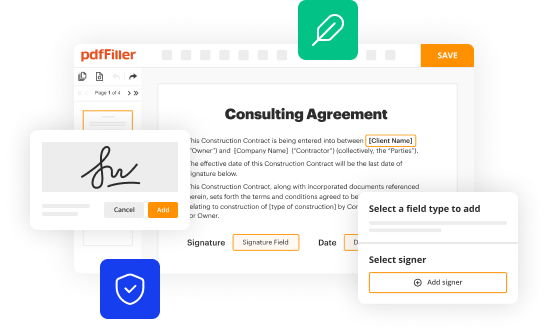
Editing history and physical form online
In order to make advantage of the professional PDF editor, follow these steps below:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit history and physical form. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
With pdfFiller, it's always easy to work with documents. Try it out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out history and physical form
How to fill out History and Physical Form
01
Gather all necessary personal information such as name, date of birth, and contact details.
02
Provide details about your medical history, including any chronic conditions and past surgeries.
03
List all medications you are currently taking, including dosages and frequency.
04
Include information about any allergies you have, particularly to medications or foods.
05
Record your family medical history, including any hereditary conditions.
06
Complete the sections pertaining to lifestyle habits, such as exercise, smoking, and alcohol consumption.
07
Sign and date the form to verify that all information is accurate and complete.
Who needs History and Physical Form?
01
Patients visiting healthcare facilities for check-ups or consultations.
02
Individuals undergoing surgery or other medical procedures.
03
New patients at a medical practice for establishing care.
04
Participants in clinical trials or research studies.
Fill
form
: Try Risk Free






People Also Ask about
How do you write a HPI?
The HPI should be written in prose with full sentences and be a narrative that builds an argument for the reason the patient was admitted. Has a starting point (i.e. “the patient was in her usual state of health until 5 days prior to admission.). Has appropriate flow, continuity, sequence, and chronologic order.
What is your HPI?
History of Present Illness (HPI) Obtaining an accurate history is the critical first step in determining the etiology of a patient's problem. A large percentage of the time, you will actually be able to make a diagnosis based on the history alone.
What is an example of HPI?
HPI notes are often used to inform emergency and admission notes so they must be able to give a complete picture of the patient's situation in a few short sentences. Example: Sudden onset of sharp chest pain, radiating to the left arm and jaw. Continuous for 2 hours and no relief with rest or antacids.
What is an example of context in HPI?
Example statements include: "fell up some stairs," "left tibia fractured while playing soccer," or "only happens when I eat green peppers." Situational stress such as "anxiety only when my ex-husband is around" qualifies for context.
What information must be included in the history and physical examination?
Documentation of the Physical Exam is typically grouped by body system, such as Head, Eyes, Ears, Nose and Throat (often abbreviated "HEENT"), Respiratory, Genito-Urinary, etc. Objective medical measurements such as blood pressure, pulse rate, temperature, etc. are made and documented.
What is the history and physical description?
The H&P: History and Physical is the most formal and complete assessment of the patient and the problem. H&P is shorthand for the formal document that physicians produce through the interview with the patient, the physical exam, and the summary of the testing either obtained or pending.
What are the 7 HPI questions?
What Questions Are Asked in an History of Present Illness? Onset. Location. Duration. Characteristics. Aggravating factors. Relieving factors. Treatments tried. Symptoms.
What is the medical history form?
Medical History Form. Record all past and/or concomitant medical conditions or surgeries. Record only one condition or surgery per line using the codes provided in the table. When recording a condition and surgery related to that condition use one line for the condition and one line for the surgery.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is History and Physical Form?
The History and Physical Form is a medical document that provides a comprehensive review of a patient's medical history and a current physical examination to guide diagnosis and treatment.
Who is required to file History and Physical Form?
Healthcare providers, such as physicians and nurse practitioners, are typically required to complete and file the History and Physical Form for patients before any surgical or certain diagnostic procedures.
How to fill out History and Physical Form?
To fill out the History and Physical Form, a healthcare provider must collect relevant patient information, including medical history, family history, medications, allergies, and perform a physical examination, then document all findings accurately on the form.
What is the purpose of History and Physical Form?
The purpose of the History and Physical Form is to ensure that healthcare providers have a complete understanding of a patient's past and present health status, which is essential for safe and effective treatment planning.
What information must be reported on History and Physical Form?
The History and Physical Form must report information such as the patient's chief complaint, medical history, surgical history, family history, medications, allergies, physical examination findings, and any pertinent diagnostic results.
Fill out your history and physical form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

History And Physical Form is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















