Get the free HISTORY AND PHYSICAL EXAMINATION FORM - uwhealth
Show details
This document serves as a comprehensive form for capturing patient's medical history, physical examination details, and assessment information during clinical evaluations.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign history and physical examination
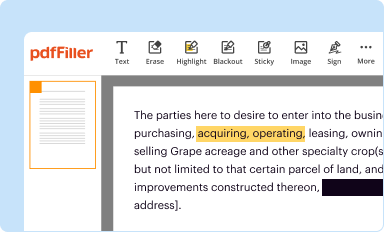
Edit your history and physical examination form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
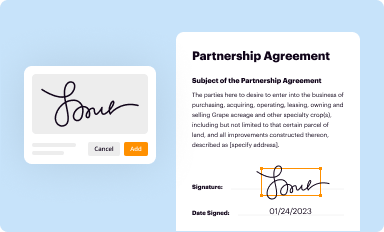
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
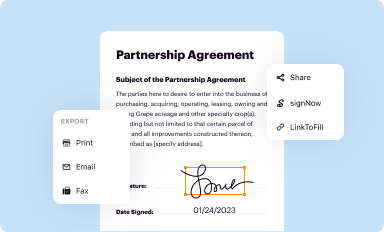
Share your form instantly
Email, fax, or share your history and physical examination form via URL. You can also download, print, or export forms to your preferred cloud storage service.
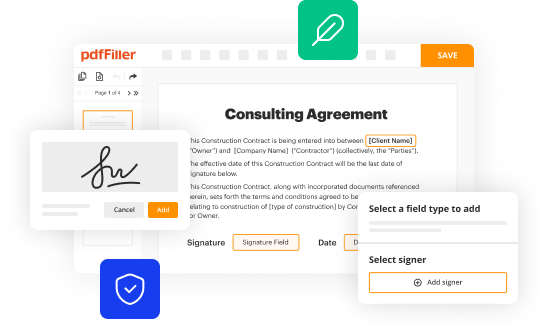
Editing history and physical examination online
Follow the steps below to benefit from the PDF editor's expertise:
1
Log into your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit history and physical examination. Replace text, adding objects, rearranging pages, and more. Then select the Documents tab to combine, divide, lock or unlock the file.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
It's easier to work with documents with pdfFiller than you can have ever thought. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out history and physical examination
How to fill out HISTORY AND PHYSICAL EXAMINATION FORM
01
Start with patient identification information: Full name, date of birth, address, and contact information.
02
Fill out the reason for the visit: Briefly state why the patient is being seen.
03
Document the patient's medical history: Include past illnesses, surgeries, and relevant family medical history.
04
Record current medications: List all medications the patient is taking, including dosages and frequency.
05
Collect vaccination history: Note any vaccinations the patient has received and their dates.
06
Perform a review of systems: Go through each body system and note any current or past issues.
07
Conduct the physical examination: Record findings from the physical examination conducted by the healthcare provider.
08
Include assessment and recommendations: Provide an assessment based on history and examination findings along with any recommendations for further evaluation or treatment.
09
Ensure all information is accurate and up to date, and sign the form.
Who needs HISTORY AND PHYSICAL EXAMINATION FORM?
01
Patients seeking medical evaluation or treatment.
02
Healthcare providers requiring a comprehensive understanding of a patient's health status.
03
Insurance companies for claims related to patient care.
04
Regulatory bodies or agencies monitoring healthcare practices.
Fill
form
: Try Risk Free






People Also Ask about
What does a physical examination include?
A physical examination usually includes: Inspection (looking at the body) Palpation (feeling the body with fingers or hands) Auscultation (listening to sounds, usually with a stethoscope)
What are the components of the focused history and physical exam?
In documenting a focused history and performing a focused physical examination, you need to explore the chief complaint, the history of the present illness, the past medical history, medications and allergies, the family history and social history, the occupational history, and the sexual history that are relevant to
How do you write a good history for a patient?
Components of a Good Medical History Patient Identification and Demographics. Chief Complaint and Presenting Symptoms. Past Medical History (PMH) Family History (FH) Social History (SH) and Lifestyle Factors. Medications and Allergies. Review of Systems (ROS)
What is included in a patient's history and physical?
The history component of an H&P gathers relevant information about the patient's history with their current chief complaint. This includes reviewing any pre-existing conditions, past hospitalizations and surgeries, allergies, medications being taken, and family medical history.
What is the history and physical exam?
We always complete a formal H&P on a new patient in the office and for admission to the hospital; it is required. Although it is called "History and Physical," it includes an assessment and plan. The assessment may be a differential diagnosis, a list of symptoms, or a problem list.
What is the HX and physical exam?
The H&P: History and Physical is the most formal and complete assessment of the patient and the problem. H&P is shorthand for the formal document that physicians produce through the interview with the patient, the physical exam, and the summary of the testing either obtained or pending.
What information must be included in the history and physical examination?
Patient age. diagnoses, the type and number of surgeries and procedures scheduled to be performed, comorbidities, and the level of anesthesia required for the surgery or procedure.
What is the format for H&P?
H & P, which stands for History of Presenting Complaint, is a format that first details the patient's current complaint in a chronological manner and then sequentially documents their medical history, examination findings, impression/diagnosis, and management plan.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is HISTORY AND PHYSICAL EXAMINATION FORM?
The History and Physical Examination Form is a document used by healthcare providers to record a patient's medical history, current health status, and findings from a physical examination.
Who is required to file HISTORY AND PHYSICAL EXAMINATION FORM?
Typically, healthcare providers such as physicians, nurses, and other medical professionals are required to file a History and Physical Examination Form, especially when admitting a patient to a healthcare facility.
How to fill out HISTORY AND PHYSICAL EXAMINATION FORM?
To fill out the History and Physical Examination Form, the healthcare provider should gather pertinent information from the patient, complete sections on medical history, physical examination findings, and any relevant assessments or plans for care.
What is the purpose of HISTORY AND PHYSICAL EXAMINATION FORM?
The purpose of the History and Physical Examination Form is to provide a comprehensive overview of a patient's health status, to assist in diagnosis, treatment planning, and to ensure continuity of care.
What information must be reported on HISTORY AND PHYSICAL EXAMINATION FORM?
The information that must be reported on the History and Physical Examination Form includes patient demographics, medical history, medication lists, allergies, review of systems, and findings from the physical examination.
Fill out your history and physical examination online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

History And Physical Examination is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.