Get the free Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® (pimecrolimus & t...
Show details
This document is a form for requesting prior authorization for Elidel® and Protopic® medications under Nevada Medicaid Managed Care. It collects patient and physician information and approval criteria.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign nevada medicaid managed care
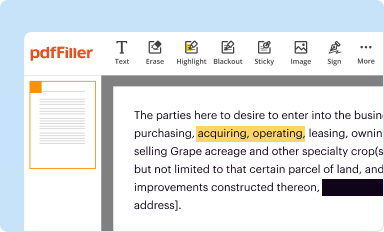
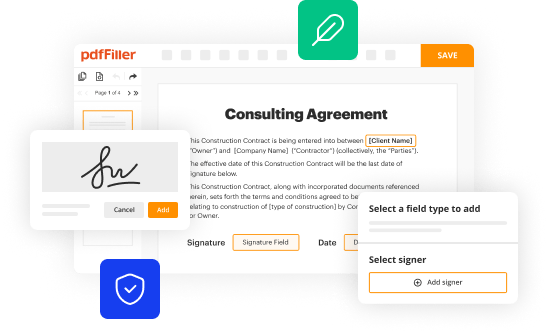
Edit your nevada medicaid managed care form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
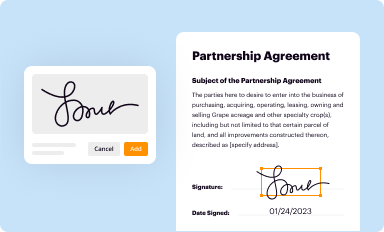
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your nevada medicaid managed care form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit nevada medicaid managed care online
To use our professional PDF editor, follow these steps:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit nevada medicaid managed care. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Save your file. Select it from your list of records. Then, move your cursor to the right toolbar and choose one of the exporting options. You can save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud, among other things.
pdfFiller makes dealing with documents a breeze. Create an account to find out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out nevada medicaid managed care
How to fill out Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® (pimecrolimus & tacrolimus) Prior Authorization of Benefits (PAB) Form
01
Obtain the Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® Prior Authorization of Benefits (PAB) Form from the official website or your healthcare provider.
02
Fill out your personal information at the top of the form, including your full name, date of birth, and Medicaid ID number.
03
Provide the information of the prescribing physician, including their name, contact information, and NPI number.
04
Detail the diagnosis and medical necessity for the use of Elidel® (pimecrolimus) or Protopic® (tacrolimus) in the appropriate section.
05
List any previous treatments tried and their outcomes if applicable.
06
Attach any necessary medical records or documentation supporting the need for the medication.
07
Review the form for completeness and accuracy before submission.
08
Submit the completed form to the appropriate Medicaid or Check Up office as specified in the instructions.
Who needs Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® (pimecrolimus & tacrolimus) Prior Authorization of Benefits (PAB) Form?
01
Individuals enrolled in Nevada Medicaid Managed Care or Nevada Check Up who require Elidel® or Protopic® for the treatment of eczema or other skin conditions.
02
Patients for whom the prescriber has determined that these treatments are medically necessary.
Fill
form
: Try Risk Free






People Also Ask about
Does Nevada Medicaid require prior authorization?
Prior authorization is necessary to ensure benefit payment. You may prescribe a health care service, treatment, equipment or medication to your patient which requires prior authorization.
Does tacrolimus need a prior authorization?
All requests for Tacrolimus Ointment require a prior authorization and will be screened for medical necessity and appropriateness using the criteria listed below.
What are the rules for Medicaid in Nevada?
Apply for Medicaid in Nevada Eligibility: The aged, blind, and disabled. Also, coverage is available if your household income is up to 138% of poverty (about $16,105 for a single person). For pregnant women, income can be up to 160%, and children are eligible for CHIP with household income up to 200% of poverty.
Does Medicare require an authorization?
Prior authorization is frequently required before Medicare Advantage plans cover a wide array of services, particularly higher cost services, including inpatient hospital stays, skilled nursing facility care, inpatient and outpatient psychiatric services, Part B drugs, and chemotherapy.
What is the phone number for Medicaid prior authorization in Nevada?
If Recipient is selected: up and call 775-687-1900. For Southern Nevada, please call 702-668-4200. If you're calling to discuss your personal care services, please call our prior authorization department at 1-800-525- 2395 o Español Lo sentimos, pero esta linea es solamente par Proveedores de servicios de salud.
What documents do I need for Medicaid in Nevada?
Proof of citizenship, such as a birth certificate or permanent residency ID card. Social Security Card. Proof of income, such as copies of your 2 most recent paystubs; if self-employed, a copy of your prior year's tax return. Current health insurance, if applicable, with ID card.
What is the FDA approved diagnosis for pimecrolimus?
chronic treatment of mild to moderate atopic dermatitis in non-immunocompromised adults and children 2 years of age and older, who have failed to respond adequately to other topical prescription treatments, or when those treatments are not advisable.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® (pimecrolimus & tacrolimus) Prior Authorization of Benefits (PAB) Form?
The Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® Prior Authorization of Benefits (PAB) Form is a document that healthcare providers must complete to request prior authorization for coverage of the medications Elidel® and Protopic® for patients enrolled in Nevada Medicaid Managed Care or Nevada Check Up programs.
Who is required to file Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® (pimecrolimus & tacrolimus) Prior Authorization of Benefits (PAB) Form?
Healthcare providers prescribing Elidel® and Protopic® for patients enrolled in Nevada Medicaid Managed Care or Nevada Check Up are required to file the Prior Authorization of Benefits (PAB) Form to obtain approval for coverage of these medications.
How to fill out Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® (pimecrolimus & tacrolimus) Prior Authorization of Benefits (PAB) Form?
To fill out the PAB Form, healthcare providers must include patient information, details about the prescribed medication (Elidel® or Protopic®), treatment history, and justification for the use of these medications, along with the provider's certification and signature. The form should be submitted according to the specific guidelines provided by the Nevada Medicaid program.
What is the purpose of Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® (pimecrolimus & tacrolimus) Prior Authorization of Benefits (PAB) Form?
The purpose of the PAB Form is to ensure that the prescribed medications Elidel® and Protopic® are medically necessary and appropriate for the patient's condition, thereby allowing for the review and approval of coverage under Nevada Medicaid Managed Care or Nevada Check Up.
What information must be reported on Nevada Medicaid Managed Care / Nevada Check Up Elidel® & Protopic® (pimecrolimus & tacrolimus) Prior Authorization of Benefits (PAB) Form?
The PAB Form must report patient demographics, prescriber information, medication details, a description of the medical condition, previous treatments tried, rationale for the requested medication, and any supporting clinical documentation that justifies the need for prior authorization.
Fill out your nevada medicaid managed care online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Nevada Medicaid Managed Care is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.