Get the free Xolair Prior Authorization of Benefits Form
Show details
This form is used to request prior authorization for the medication Xolair (omalizumab) for patients with moderate to severe persistent asthma and concurrent allergic rhinitis, outlining the required
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign xolair prior authorization of
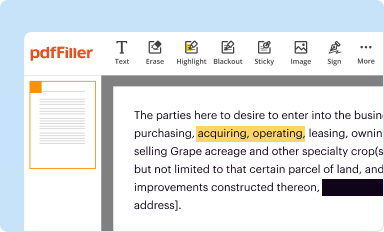
Edit your xolair prior authorization of form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
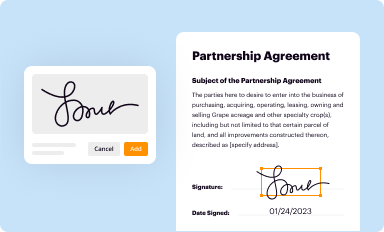
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
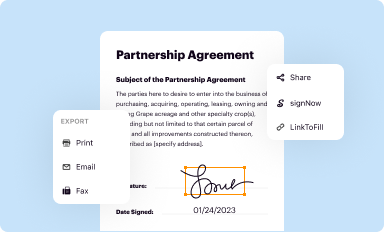
Share your form instantly
Email, fax, or share your xolair prior authorization of form via URL. You can also download, print, or export forms to your preferred cloud storage service.
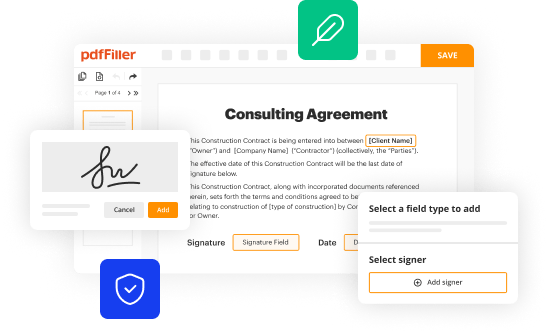
Editing xolair prior authorization of online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit xolair prior authorization of. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
Dealing with documents is always simple with pdfFiller.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out xolair prior authorization of
How to fill out Xolair Prior Authorization of Benefits Form
01
Obtain the Xolair Prior Authorization of Benefits Form from your healthcare provider or insurance company.
02
Fill in the patient's personal information, including name, date of birth, and insurance details.
03
Provide the physician's information, including name, contact number, and NPI number.
04
Include details of the patient's medical history relevant to the use of Xolair.
05
Specify the diagnosis or condition for which Xolair is being prescribed.
06
List other treatments tried or considered before prescribing Xolair.
07
Indicate the prescribed dosage and frequency of Xolair administration.
08
Sign and date the form, affirming that the information provided is accurate.
09
Submit the completed form to the insurance company via the preferred submission method (fax, mail, or online).
10
Follow up with the insurance provider to confirm receipt and approval status.
Who needs Xolair Prior Authorization of Benefits Form?
01
Patients diagnosed with moderate to severe asthma who are inadequately controlled on other medications.
02
Individuals with chronic idiopathic urticaria (hives) that do not respond to antihistamines.
03
Patients with nasal polyps associated with asthma as part of their treatment plan.
04
Anyone requiring insurance coverage for Xolair to ensure affordability and access to the medication.
Fill
form
: Try Risk Free






People Also Ask about
How to get approved for XOLAIR?
Patient selection, determined by the healthcare provider in consultation with the patient, should take into account the pattern of anaphylaxis events seen in premarketing clinical trials and postmarketing spontaneous reports, as well as individual patient risk factors (e.g. prior history of anaphylaxis), ability to
Is XOLAIR covered by insurance?
For patients with commercial insurance, about 55% of patients paid $0 out-of-pocket costs per month for XOLAIR. For those patients who did have out-of-pocket costs, 90% paid between $5 to $1,475 per month, after satisfying their deductible. The amount you pay for XOLAIR will depend on your insurance plan.
What forms does XOLAIR come in?
Xolair comes in three forms: a syringe prefilled with solution, an autoinjector prefilled with solution, and a vial of powdered medication. (A healthcare professional mixes the powder into a solution.) Both forms are for subcutaneous injection, which is given under the skin.
Does Opzelura require prior authorization?
As with other Janus kinase (JAK) inhibitors, most health plans require a prior authorization (PA) before approving coverage for OPZELURA. The patient must be 12 years of age or older. OPZELURA is indicated for: Mild to moderate atopic dermatitis.
What are three drugs that require prior authorization?
Drugs That May Require Prior Authorization Drug ClassDrugs in Class Epidiolex Epidiolex Erythroid Stimulants , , Procrit and Retacrit, Mircera Esbriet Esbriet Evenity Evenity242 more rows
Does XOLAIR require prior authorization?
All requests for Xolair (omalizumab) require a prior authorization and will be screened for medical necessity and appropriateness using the criteria listed below.
What is the XOLAIR financial assistance program?
With the XOLAIR Co-pay Program, eligible patients with commercial insurance may pay as little as $0 XOLAIR drug out-of-pocket cost. The program covers up to $15,000 per calendar year benefit period. Note: The final amount owed may be as little as $0, but may vary depending on the health insurance plan.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Xolair Prior Authorization of Benefits Form?
The Xolair Prior Authorization of Benefits Form is a document that healthcare providers submit to obtain approval from insurance companies before prescribing Xolair, a medication used to treat conditions like asthma and chronic hives.
Who is required to file Xolair Prior Authorization of Benefits Form?
Healthcare providers, such as doctors or allergists, who prescribe Xolair for their patients are required to file the Prior Authorization of Benefits Form.
How to fill out Xolair Prior Authorization of Benefits Form?
To fill out the Xolair Prior Authorization of Benefits Form, providers must provide patient information, details of the proposed treatment, relevant medical history, and justification for the use of Xolair. It's important to follow the specific guidelines provided by the insurance company.
What is the purpose of Xolair Prior Authorization of Benefits Form?
The purpose of the Xolair Prior Authorization of Benefits Form is to ensure that the prescribed treatment is medically necessary and to obtain approval for coverage from the patient's insurance provider.
What information must be reported on Xolair Prior Authorization of Benefits Form?
The information that must be reported includes the patient's personal details, diagnosis, treatment plan, previous medications tried, medical history, and the rationale for prescribing Xolair.
Fill out your xolair prior authorization of online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Xolair Prior Authorization Of is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.