
Get the free Out-Of-Network Claim Form
Show details
This form is used by members of Vision Care plans to claim reimbursement for services received from out-of-network vision care providers.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign out-of-network claim form
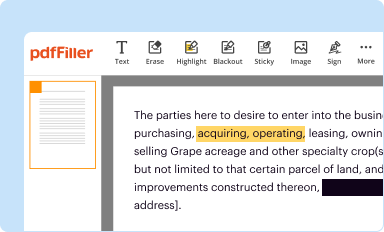
Edit your out-of-network claim form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
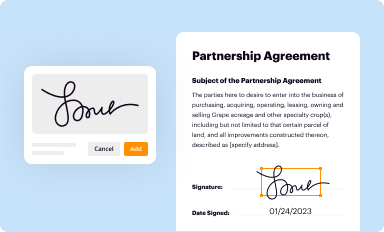
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
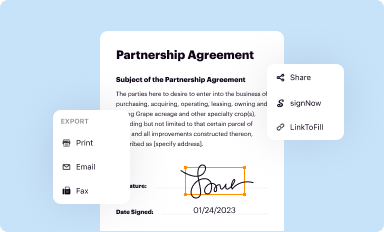
Share your form instantly
Email, fax, or share your out-of-network claim form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
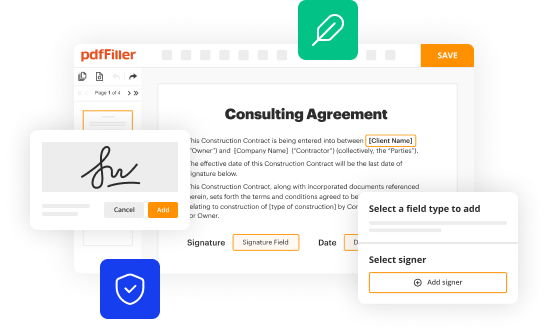
Editing out-of-network claim form online
Follow the steps below to take advantage of the professional PDF editor:
1
Log in to account. Click Start Free Trial and sign up a profile if you don't have one.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit out-of-network claim form. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
Dealing with documents is simple using pdfFiller.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out out-of-network claim form
How to fill out Out-Of-Network Claim Form
01
Obtain the Out-Of-Network Claim Form from your insurance provider's website or customer service.
02
Fill in your personal information including name, address, policy number, and contact details.
03
Provide details of the healthcare provider including their name, address, and the services rendered.
04
Attach any necessary documentation such as itemized bills, receipts, and medical records to support your claim.
05
Review the completed form for accuracy and completeness.
06
Sign and date the form to certify that all information is true.
07
Submit the claim form along with the attached documents to the address provided by your insurance company.
Who needs Out-Of-Network Claim Form?
01
Individuals who have received medical services from an out-of-network provider.
02
Patients whose insurance does not cover certain services or providers in-network.
03
Policyholders seeking reimbursement for medical expenses incurred outside of their insurance network.
Fill
form
: Try Risk Free






People Also Ask about
How do I write an appeal for an out-of-network claim?
How to write an appeal letter to insurance company appeals departments Step 1: Gather Relevant Information. Step 2: Organize Your Information. Step 3: Write a Polite and Professional Letter. Step 4: Include Supporting Documentation. Step 5: Explain the Error or Omission. Step 6: Request a Review. Step 7: Conclude the Letter.
What is an example of a reason for appeal?
When appealing against a guilty verdict a defendant might say: there was something unfair about the way their trial took place. a mistake was made in their trial. the verdict could not be sustained on the evidence.
What is an out-of-network claim?
When a plan and provider do not participate in the same network – or if either party is not a part of any network – then resulting claims are considered Out-of-Network, and patients will be responsible for paying the portion of the provider's charges that exceed the plan's Allowed Amount.
How do I submit an out of network claim to VSP?
But, if you go out-of-network, you can submit a claim for reimbursement online from your VSP member account or by contacting VSP Member Services at 800.877.7195 and requesting a claim/reimbursement form.
How do I write an insurance appeal letter out of the network?
Things to Include in Your Appeal Letter Patient name, policy number, and policy holder name. Accurate contact information for patient and policy holder. Date of denial letter, specifics on what was denied, and cited reason for denial. Doctor or medical provider's name and contact information.
What do you say when appealing an insurance claim?
To Whom It May Concern: I am writing to request a review of your denial of the claim for treatment or services provided by name of provider on date provided. The reason for denial was listed as (reason listed for denial), but I have reviewed my policy and believe treatment or service should be covered.
How do you write a powerful appeal letter?
Content and Tone Opening Statement. The first sentence or two should state the purpose of the letter clearly. Be Factual. Include factual detail but avoid dramatizing the situation. Be Specific. Documentation. Stick to the Point. Do Not Try to Manipulate the Reader. How to Talk About Feelings. Be Brief.
How does out of network work with VSP?
Yes. If VSP out-of-network coverage is included in your plan, members can obtain services from any provider they choose, including national or retail chains. Reimbursement for out-of- network services is ing to a schedule with the same copays and limitations as services through VSP network providers.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Out-Of-Network Claim Form?
An Out-Of-Network Claim Form is a document that policyholders use to request reimbursement for medical services received from healthcare providers who do not belong to their insurance network.
Who is required to file Out-Of-Network Claim Form?
Policyholders who receive medical services from out-of-network providers and wish to claim reimbursement for those services are required to file an Out-Of-Network Claim Form.
How to fill out Out-Of-Network Claim Form?
To fill out the Out-Of-Network Claim Form, individuals should provide personal information, details of the medical services received, including dates, costs, and the provider's information, and submit any supporting documentation such as receipts and invoices.
What is the purpose of Out-Of-Network Claim Form?
The purpose of the Out-Of-Network Claim Form is to facilitate the process of obtaining reimbursement from an insurance provider for medical expenses incurred from non-network healthcare providers.
What information must be reported on Out-Of-Network Claim Form?
The information that must be reported on the Out-Of-Network Claim Form includes the policyholder's name, insurance policy number, details of the out-of-network provider, descriptions of the services rendered, dates of service, and itemized billing statements.
Fill out your out-of-network claim form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Out-Of-Network Claim Form is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















