Get the free Pharmacy Utilization Management Programs for 2004
Show details
This document outlines the utilization management programs implemented by Blue Cross and Blue Shield of Kansas for 2004, focusing on managing prescription drug usage to enhance outcomes and reduce
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign pharmacy utilization management programs
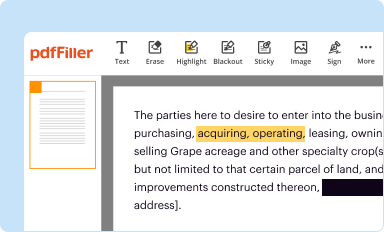
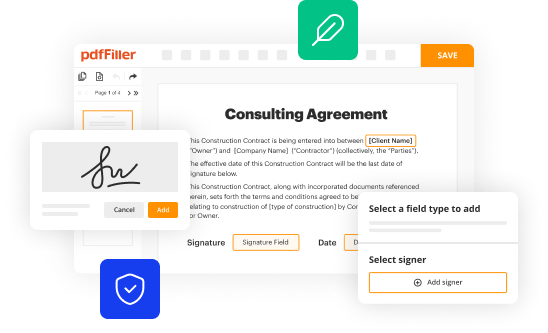
Edit your pharmacy utilization management programs form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
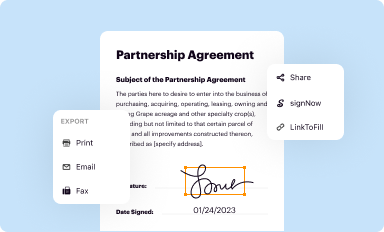
Share your form instantly
Email, fax, or share your pharmacy utilization management programs form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing pharmacy utilization management programs online
Follow the steps down below to use a professional PDF editor:
1
Check your account. In case you're new, it's time to start your free trial.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit pharmacy utilization management programs. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
It's easier to work with documents with pdfFiller than you could have believed. Sign up for a free account to view.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out pharmacy utilization management programs
How to fill out Pharmacy Utilization Management Programs for 2004
01
Gather all relevant patient information including demographics, prescription history, and diagnosis.
02
Review the Pharmacy Utilization Management Programs guidelines and requirements for 2004.
03
Complete the required sections, including patient eligibility, medication details, and prescribing information.
04
Provide any necessary supporting documentation, such as lab results or prior authorizations.
05
Submit the filled-out form by the specified deadline to the appropriate pharmacy management organization.
06
Keep copies of all submitted documents for your records and follow up to confirm receipt.
Who needs Pharmacy Utilization Management Programs for 2004?
01
Healthcare providers who prescribe medications.
02
Pharmacists involved in medication management.
03
Healthcare organizations aiming to control prescription drug costs.
04
Patients who require prior authorization for their medications.
05
Insurance companies managing pharmacy benefits.
Fill
form
: Try Risk Free






People Also Ask about
What is the utilization review process?
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
What is um in pbm?
Utilization management (UM) is a process that is part of your health plan. Utilization management helps to make sure that you are getting the right drugs -- all while helping to make medicine more affordable.
What is UM in packaging?
The "µ" symbol means micro (it's also the twelfth letter of the Greek alphabet). So 1µm is one millionth of a metre, or one thousandth of a millimetre. That's very small! In the packaging industry, this measurement is commonly used for the thickness of plastics.
What are the tools of drug utilization management?
Utilization management tools, such as prior authorization, quantity limits and step therapy, apply to select drugs to ensure safe and cost-effective use of drugs on the plan's drug list.
What is UM in pharma?
Utilization management (UM) is a process that is part of your health plan. Utilization management helps to make sure that you are getting the right drugs -- all while helping to make medicine more affordable.
What does UM mean in medical insurance?
A utilization management (UM) policy is a document containing clinical criteria used by Medica staff members for prior authorization, appropriateness of care determination and coverage. The criteria are specific to the clinical characteristics of the population that will benefit from the treatment or technology.
What is utilization and case management?
Interplay Between Case Management and Utilization Review Case management identifies patients who require specialized attention, while UR ensures that the care provided is necessary and at the most appropriate level.
What is UM in copywriting?
"Like" and "um" as well as other word fillers, can be used to great effect to show uncertainty in a characters dialogue. So I would make sure that you know exactly what tone you wish to display to your reading audience. Word fillers can also be useful character quirks.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Pharmacy Utilization Management Programs for 2004?
Pharmacy Utilization Management Programs for 2004 refer to a set of guidelines and policies designed to optimize the use of prescription medications in patient care. These programs aim to ensure that patients receive the most appropriate, effective, and cost-efficient drug therapy.
Who is required to file Pharmacy Utilization Management Programs for 2004?
Pharmacy benefit managers (PBMs), health plans, and insurance providers are typically required to file Pharmacy Utilization Management Programs for 2004. They must comply with regulations set forth by state and federal guidelines.
How to fill out Pharmacy Utilization Management Programs for 2004?
Filling out the Pharmacy Utilization Management Programs for 2004 requires gathering relevant data about medication utilization, applying specific criteria for drug selection and approval, and documenting the outcomes of the program as per the prescribed format provided by regulatory bodies.
What is the purpose of Pharmacy Utilization Management Programs for 2004?
The purpose of Pharmacy Utilization Management Programs for 2004 is to improve patient care by managing drug utilization effectively, reducing unnecessary costs, preventing medication errors, and ensuring access to effective therapies.
What information must be reported on Pharmacy Utilization Management Programs for 2004?
Information that must be reported includes drug utilization statistics, criteria used for approval or denial of medications, cost-effectiveness analyses, patient outcomes, and compliance with regulations.
Fill out your pharmacy utilization management programs online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Pharmacy Utilization Management Programs is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.