
Get the free Request for Redetermination of Medicare Prescription Drug Denial
Show details
This document provides information for enrollees on how to appeal a denial of Medicare prescription drug coverage, including instructions for submitting a redetermination request.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign request for redetermination of
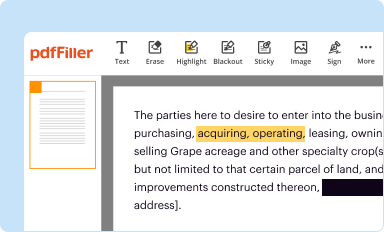
Edit your request for redetermination of form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
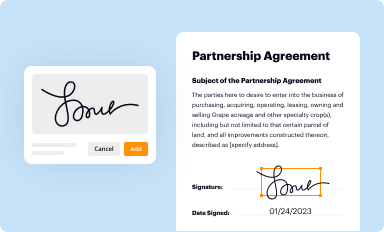
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
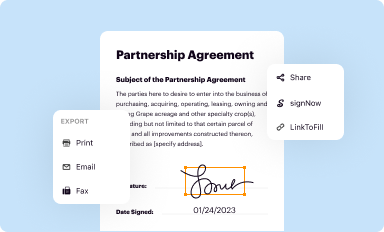
Share your form instantly
Email, fax, or share your request for redetermination of form via URL. You can also download, print, or export forms to your preferred cloud storage service.
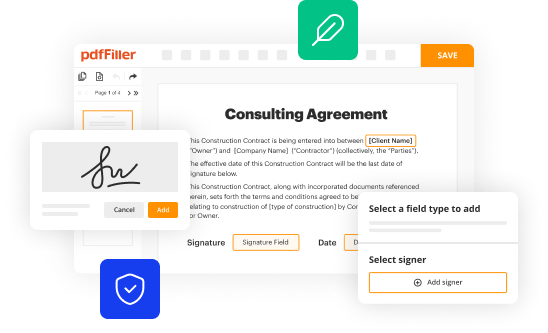
How to edit request for redetermination of online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit request for redetermination of. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
It's easier to work with documents with pdfFiller than you can have ever thought. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out request for redetermination of
How to fill out Request for Redetermination of Medicare Prescription Drug Denial
01
Obtain the Request for Redetermination form from the Medicare website or your Medicare plan provider.
02
Fill in your personal information, including your name, Medicare number, and contact details.
03
Clearly state the reason for the denial of your Medicare prescription drug coverage.
04
Include any supporting documents, such as medical records or notes from your healthcare provider, that justify your need for the prescribed medication.
05
Sign and date the form to certify that the information provided is accurate and complete.
06
Submit the completed form and any attachments to the address provided by your Medicare plan within 60 days of receiving the denial notice.
Who needs Request for Redetermination of Medicare Prescription Drug Denial?
01
Individuals whose Medicare prescription drug claims have been denied.
02
Beneficiaries seeking coverage for medications that are deemed non-covered or not medically necessary.
03
Patients needing to appeal a decision about their prescription drug coverage.
Fill
form
: Try Risk Free






People Also Ask about
What is a medicare part D redetermination?
Redetermination by the Part D Plan Sponsor. If a Part D plan sponsor denies an enrollee's request, in whole or in part, the enrollee, the enrollee's prescriber, or the enrollee's representative may appeal the decision to the plan sponsor by requesting a standard or expedited redetermination.
What is the best way to win a Medicare appeal?
What is the best way to win a Medicare appeal? Make sure all notices from Medicare or the Medicare Advantage plan are fully read and understood. Include a letter from the beneficiary's doctor in support of the appeal. Make sure to meet appeal deadlines. Keep a copy of all documents sent and received during the process.
How do I appeal a Medicare prescription denial?
You, your representative, or your prescriber must ask for an appeal within 65 days from the date on the initial denial notice sent by your plan. If you miss the deadline, you must give a reason for filing late. Include this information in your appeal: Your name, address, and the Medicare Number on your Medicare card.
How do you win a prescription appeal?
Include any treatments or therapies you've tried and facts that offset the reason your claim was denied. Discuss what will happen to your condition without the treatment. Include supporting evidence, such as peer-reviewed journal articles or treatment guidelines from recognized organizations.
What percentage of medicare appeals are successful?
The vast majority of denied prior authorization requests that were appealed were subsequently overturned by Medicare Advantage insurers. From 2019 through 2023, more than eight in ten (81.7%) denied prior authorization requests that were appealed were overturned (Figure 5).
Why did Medicare deny my prescription?
If your plan made an error, they should correct it. If not, there are a few common reasons a plan may deny payment: Prior authorization: you must get prior approval from the plan before it will cover a specific drug. Step therapy: your plan requires you try a different or less expensive drug first.
What is the fax number for Medicare Tier exception form?
Completed forms should be faxed to: 800-693-6703. It is not necessary to fax this cover page. Use this form to request coverage of a brand or generic in a higher cost sharing tier at a lower cost sharing tier. Certain restrictions apply**.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Request for Redetermination of Medicare Prescription Drug Denial?
A Request for Redetermination is a formal appeal filed by a Medicare beneficiary to contest the denial of coverage for a prescribed medication under Medicare Part D.
Who is required to file Request for Redetermination of Medicare Prescription Drug Denial?
The Medicare beneficiary or their authorized representative is required to file a Request for Redetermination.
How to fill out Request for Redetermination of Medicare Prescription Drug Denial?
To fill out the Request for Redetermination, beneficiaries must gather their Medicare details, include information about the denied drug, provide reasons for the appeal, and submit the completed form to the appropriate Medicare plan.
What is the purpose of Request for Redetermination of Medicare Prescription Drug Denial?
The purpose is to allow beneficiaries to challenge a denial of coverage for a particular medication, seeking a review of the decision that led to the denial.
What information must be reported on Request for Redetermination of Medicare Prescription Drug Denial?
The information includes the beneficiary's personal details, details of the denied medication, the reason for the denial, and any supporting documentation that substantiates the claim for coverage.
Fill out your request for redetermination of online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Request For Redetermination Of is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















