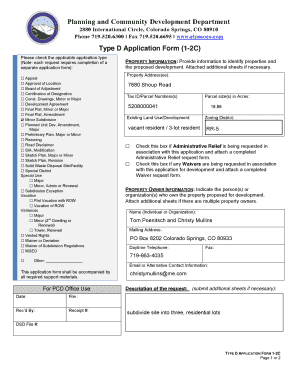
Get the free COBRA Administration
Show details
This document outlines the COBRA administration services offered by Blue Cross of Idaho, including details on coverage continuation for former employees and associated responsibilities for employers.
We are not affiliated with any brand or entity on this form
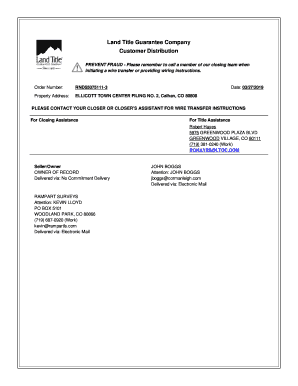
Get, Create, Make and Sign cobra administration
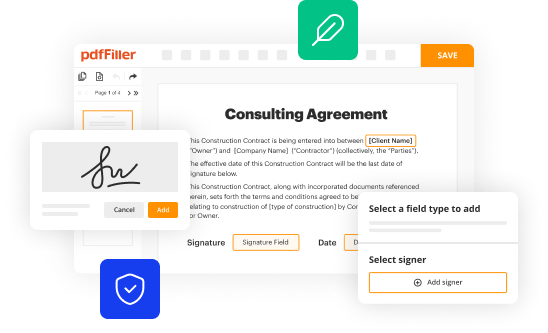
Edit your cobra administration form online
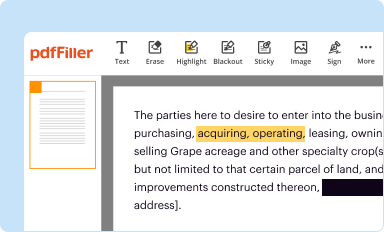
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
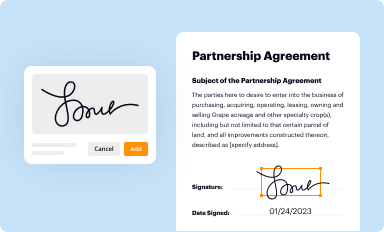
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
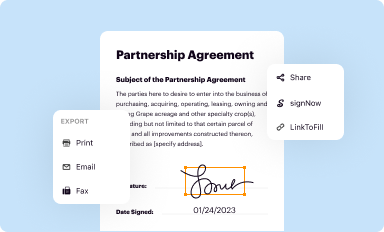
Share your form instantly
Email, fax, or share your cobra administration form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing cobra administration online
To use our professional PDF editor, follow these steps:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit cobra administration. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
With pdfFiller, dealing with documents is always straightforward.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out cobra administration
How to fill out COBRA Administration
01
Collect all necessary employee information, including full name, address, and Social Security number.
02
Determine the qualifying event that triggers COBRA eligibility (e.g., termination, reduction in hours, etc.).
03
Notify eligible employees and their dependents of their COBRA rights within the required timeframe.
04
Provide detailed information about the health insurance plan, coverage options, premiums, and deadlines.
05
Make sure to inform employees how to elect COBRA coverage and any payment requirements.
06
Set up a system to track COBRA elections and payments made by employees.
Who needs COBRA Administration?
01
Employees who work for a company with 20 or more employees and have experienced a qualifying event that affects their health insurance coverage.
02
Dependents of eligible employees who are also affected by the qualifying event.
03
Employers who are required to provide COBRA coverage as part of federal law.
Fill
form
: Try Risk Free






People Also Ask about
What is the purpose of a COBRA?
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
What does COBRA stand for?
COBRA stands for Consolidated Omnibus Budget Reconciliation Act. This is the federal law that provides many workers with the right to continue coverage in a group health plan. This federal law applies to employers with 20 or more employees, including self-insured employers.
What is a COBRA admin?
A COBRA plan administrator is responsible for effectively recording, tracking, and overseeing the necessary steps for a business to comply with COBRA law.
How to get in contact with COBRA?
Call 1-866-444-3272. You may qualify to keep your health coverage with COBRA. Call today.
What does COBRA mean in benefits?
COBRA, the Consolidated Omnibus Budget Reconciliation Act, lets qualified workers keep their group health insurance for a limited time after a change in eligibility.
What does COBRA mean in business?
COBRA, the Consolidated Omnibus Budget Reconciliation Act, lets qualified workers keep their group health insurance for a limited time after a change in eligibility.
Who is your COBRA administrator?
Who Is My COBRA Administrator? Your COBRA Administrator maybe someone in the employer's human resources department from which the insurance is through. Though, some companies will use a third-party administrator, also known as a TPA, to manage health insurance continuation plans.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is COBRA Administration?
COBRA Administration refers to the process of managing the COBRA health insurance continuation program, which allows employees and their families to continue health insurance coverage for a limited time after a qualifying event, such as job loss or reduction in work hours.
Who is required to file COBRA Administration?
Employers with 20 or more employees who offer group health plans are required to comply with COBRA and must administer COBRA coverage for eligible employees and their dependents.
How to fill out COBRA Administration?
To fill out COBRA Administration, employers must notify eligible participants about their rights under COBRA, provide necessary forms, document eligible events, and report the continuation of coverage to the relevant health insurance providers.
What is the purpose of COBRA Administration?
The purpose of COBRA Administration is to ensure that employees and their families have the opportunity to maintain their health insurance coverage even after experiencing a qualifying life event, thus protecting their access to healthcare.
What information must be reported on COBRA Administration?
The information that must be reported in COBRA Administration includes details about the qualifying event, the names of covered individuals, the duration of coverage, premium amounts, and any changes to coverage options.
Fill out your cobra administration online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Cobra Administration is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.