Get the free Model COBRA Continuation Coverage Supplemental Notice
Show details
This document provides important information regarding the availability of COBRA premium reduction under the American Recovery and Reinvestment Act of 2009 for qualified beneficiaries who lost health
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign model cobra continuation coverage
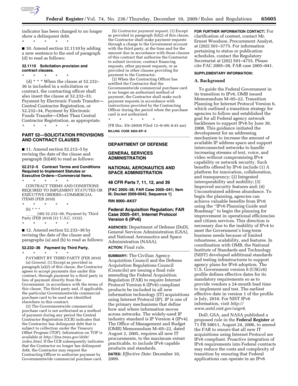
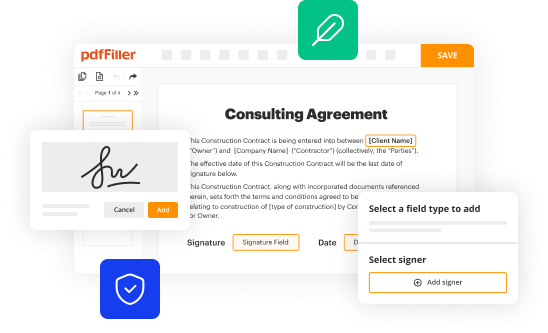
Edit your model cobra continuation coverage form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your model cobra continuation coverage form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit model cobra continuation coverage online
Follow the steps below to benefit from the PDF editor's expertise:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit model cobra continuation coverage. Replace text, adding objects, rearranging pages, and more. Then select the Documents tab to combine, divide, lock or unlock the file.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
With pdfFiller, it's always easy to deal with documents. Try it right now
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out model cobra continuation coverage
How to fill out Model COBRA Continuation Coverage Supplemental Notice
01
Obtain the Model COBRA Continuation Coverage Supplemental Notice from the Department of Labor website or your employer.
02
Read through the notice to understand the information required.
03
Fill in the necessary details, including the name of the plan, the name of the participant, and any relevant dates.
04
Ensure you include specific information regarding the coverage options available, premiums, and deadlines.
05
Check for any required signatures or additional documentation that might be needed.
06
Review the completed notice for accuracy before submission.
Who needs Model COBRA Continuation Coverage Supplemental Notice?
01
Employers who offer group health plans.
02
Employees and their dependents who may be eligible for COBRA continuation coverage after a qualifying event.
Fill
form
: Try Risk Free






People Also Ask about
Why did I get a continuation coverage right under COBRA?
Failing to adhere to COBRA rules can result in costly penalties. The Department of Labor may impose fines of $110 per day per qualified beneficiary for non-compliance with notice requirements, and the IRS can levy excise taxes for violations.
Is COBRA continuation coverage worth it?
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
What is the 60 day COBRA loophole?
You have 60 days to enroll in COBRA once your employer-sponsored benefits end. Even if your enrollment is delayed, you will be covered by COBRA starting the day your prior coverage ended.
Why did I get a COBRA continuation letter?
Strict legal requirements govern when many employers must send COBRA continuation notices to their employees. Employers are often required to send notifications (or have them sent by a plan administrator) when employees experience qualifying events — which can include a reduction in hours or termination.
What are the disadvantages of COBRA coverage?
COBRA cons COBRA can be expensive, especially compared to the premiums you were paying before your qualifying event. COBRA does not apply to all employer-sponsored health plans — in particular, those organizations with fewer than 20 employees may have no requirements. Even if you get an extension, COBRA is only temporary.
Why am I getting a letter about COBRA coverage?
The COBRA notification may come from your former employer or a third-party administrator that will manage that plan moving forward. Your COBRA election notice will contain all of the information you will need to continue your health plan.
How does COBRA continuation coverage work?
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
What is a continuation COBRA?
After you leave employment, you and/or your covered dependents may be eligible to continue health insurance coverage under COBRA for up to 18 months. Your COBRA continuation coverage is limited to the medical, dental and/or vision benefits you had when you left employment.
What is COBRA continuation rights?
Federal COBRA is a federal law that lets you keep your group health plan when your job ends or your hours are cut. Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children.
Is cobra insurance worth getting?
If your medical expenses are going to be more than the COBRA premiums and you are close to meeting your deductible or out-of-pocket maximum, then it might be worth it to stay on COBRA.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Model COBRA Continuation Coverage Supplemental Notice?
The Model COBRA Continuation Coverage Supplemental Notice is a standard notice provided to individuals eligible for COBRA benefits, outlining their rights and options for continuing healthcare coverage after employment ends or other qualifying events.
Who is required to file Model COBRA Continuation Coverage Supplemental Notice?
Employers who offer group health plans and are subject to COBRA requirements are required to provide the Model COBRA Continuation Coverage Supplemental Notice to qualified beneficiaries.
How to fill out Model COBRA Continuation Coverage Supplemental Notice?
To fill out the Model COBRA Continuation Coverage Supplemental Notice, employers should include specific details about the health plan, coverage options, premium costs, payment procedures, and the rights of eligible employees.
What is the purpose of Model COBRA Continuation Coverage Supplemental Notice?
The purpose of the Model COBRA Continuation Coverage Supplemental Notice is to inform qualified beneficiaries of their rights to continue health insurance coverage under COBRA and to provide them with necessary information regarding enrollment and costs.
What information must be reported on Model COBRA Continuation Coverage Supplemental Notice?
The information that must be reported includes the name of the group health plan, identification of the qualifying event, the dates of coverage, the premium amount, payment deadlines, and contact information for further inquiries.
Fill out your model cobra continuation coverage online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Model Cobra Continuation Coverage is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.