Get the free medigold prior authorization form
Fill out, sign, and share forms from a single PDF platform
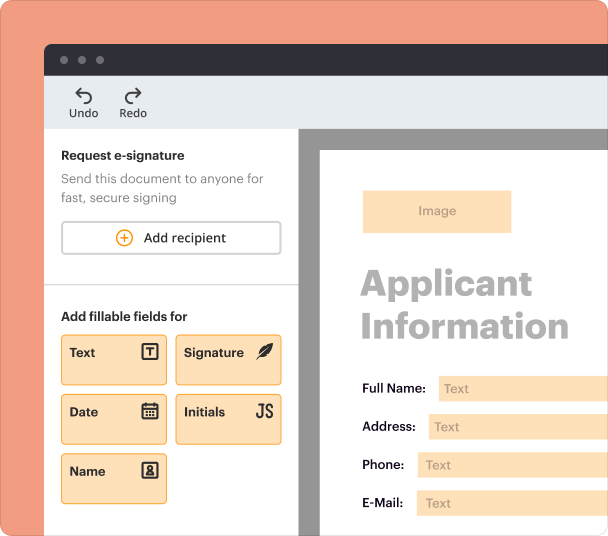
Edit and sign in one place
Create professional forms
Simplify data collection
Manage forms centrally
Why pdfFiller is the best tool for your documents and forms
End-to-end document management
Accessible from anywhere
Secure and compliant
Guide to Medigold Prior Authorization Form Management
How does prior authorization work?
Prior authorization is a healthcare process where a provider obtains permission from a patient's insurance before administering certain treatments or medications. This helps ensure that the proposed care is medically necessary and within the scope of the patient's insurance coverage. In the case of Medigold, the prior authorization process is integral to managing healthcare costs and enhancing patient outcomes.
-
Prior authorization serves to verify that a proposed treatment is in line with the patient's medical needs, helping to control costs for insurers.
-
It fosters communication between healthcare providers and insurers, ensuring that treatment plans align with coverage.
-
Prior authorization must adhere to regulations to protect patient data and uphold insurance agreements.
-
Medigold assists members by offering streamlined prior authorization processes and support resources.
Where can access the Medigold prior authorization form?
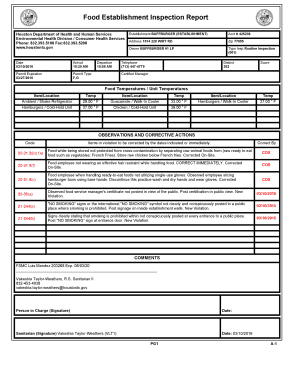
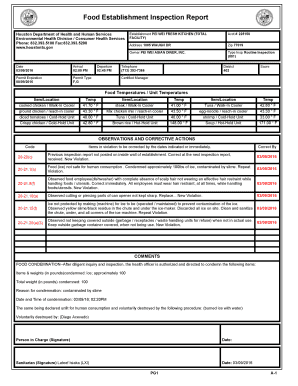
The Medigold Prior Authorization Form can be conveniently accessed on pdfFiller, a cloud-based solution that allows users to handle documents seamlessly. This platform simplifies the downloading process while providing a clear layout of the form.
-
By navigating to the relevant section, you can locate and access the Medigold prior authorization form quickly.
-
Use the search feature on pdfFiller, enter 'Medigold prior authorization form', and follow the prompts to download it easily.
-
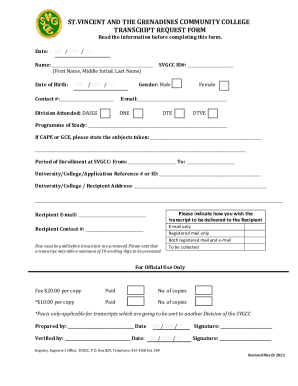
The form typically includes sections for patient details, medical history, and necessary treatment information.
What are the steps to fill out the Medigold prior authorization form?
Filling out the Medigold prior authorization form requires attention to detail and accuracy. Each section is designed to gather essential information relevant to the requested treatment, and following detailed instructions can help ensure a smooth submission.
-
Ensure you read the guidelines carefully, as each part asks for specific information necessary for review.
-
You will need to provide information about patient consent for treatment, a brief medical history, and if applicable, details about the employer.
-
Double-check all entries for accuracy to avoid delays in the authorization process.
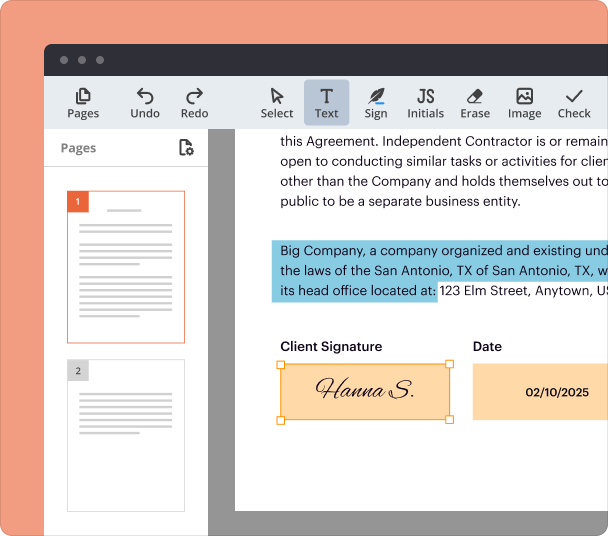
How can edit and sign the form on pdfFiller?
pdfFiller's platform offers user-friendly editing tools, allowing you to make necessary modifications to the Medigold prior authorization form. Additionally, applying digital signatures has never been easier, ensuring your document is legally binding.
-
Edit fields directly or add notes where needed, providing a detailed and customized form.
-
With pdfFiller, a signature can be added electronically, maintaining the authenticity of your submission.
-
Invite others to view or edit the form collaboratively, making it easier to gather necessary approvals.
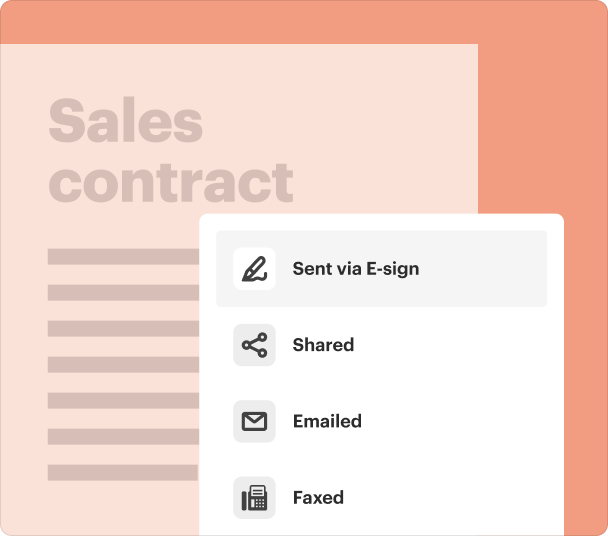
What are the methods for submitting the completed form?
Understanding submission methods for the Medigold prior authorization form is crucial to ensuring timely processing. You have choices between digital and print submissions, each varying in terms of convenience and compliance.
-
Digital submissions through pdfFiller are generally faster, whereas print submissions may require additional postal time.
-
Ensure to follow all guidelines set by Medigold regarding confidentiality and proper handling of patient information.
-
Keep a record of your submission and regularly check the status to ensure timely approvals.
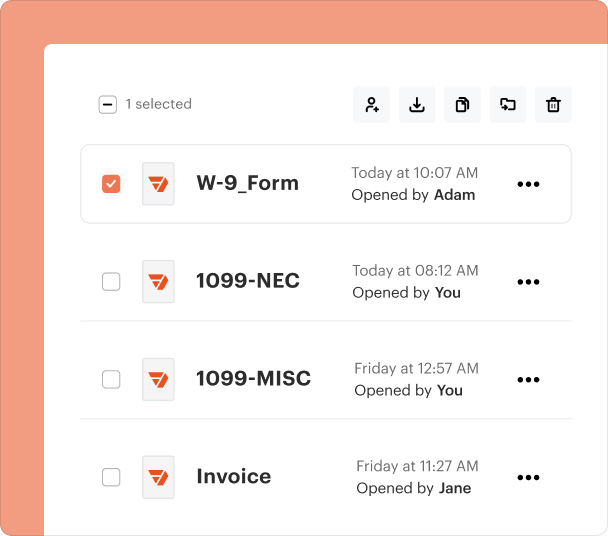
How can manage authorized documents on pdfFiller?
Managing documents within pdfFiller efficiently can save time and streamline your workflow. It’s essential to adopt best practices for document organization and storage, maximizing the platform’s capabilities.
-
Use regular naming conventions and folders for easy retrieval of the Medigold prior authorization form and related documents.
-
Take advantage of the cloud to access your documents from anywhere, ensuring you’re always prepared.
-
Implement a tagging system to help you locate and manage various healthcare documents effectively.
What are the legal aspects of prior authorization?
Understanding the legal landscape surrounding prior authorization is vital for both patients and healthcare providers. Key regulations help secure patient rights and ensure compliance with medical reporting standards.
-
This act governs the handling and consent processes for medical reports, protecting patient rights.
-
It is essential to protect sensitive information shared within consent forms and follow applicable data protection regulations.
-
Compliance with these regulations affects how patients receive care and how employers manage employee health insurance.
Conclusion & importance of staying informed
Staying updated on forms and regulations related to the Medigold prior authorization process is vital for ensuring seamless healthcare management. Regularly checking for updates and leveraging resources from healthcare professionals can empower individuals to navigate the complexities involved effectively.
Frequently Asked Questions about medigold prior authorization form
What is the purpose of the Medigold prior authorization form?
The form is designed to obtain prior approval for specific treatments or medications to ensure they are necessary and covered by insurance. It streamlines the authorization process for both healthcare providers and patients.
How long does it take to get approval after submitting the form?
Approval times can vary widely depending on the complexity of the request and the insurance provider's internal processes. Typically, you can expect a response within a few days to a week.
Can I submit more than one prior authorization request at a time?
Yes, you can submit multiple requests, but ensure that all necessary information is accurately provided for each request to avoid any delays in processing.
What should I do if my prior authorization is denied?
If your request is denied, carefully review the reason for the denial, and consider appealing the decision. Consulting with your healthcare provider can help clarify next steps.
Is it necessary to sign the form before submission?
Yes, signing the form confirms your consent for the requested treatment and is a crucial part of the submission to comply with regulatory requirements.
pdfFiller scores top ratings on review platforms