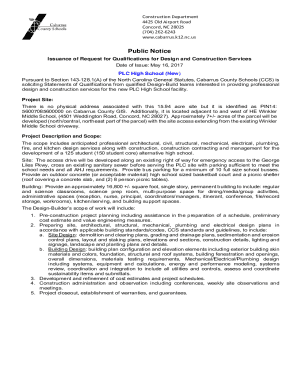
Anthem Form 94044 2003-2026 free printable template
Show details
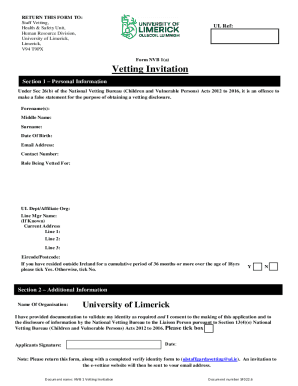
THIS SECTION MUST BE COMPLETED Employee Member Number Health Group Number Dental Group Number Vision Group Number COBRA or State Continuation of Coverage Application Continuation of Medical, Dental
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign Anthem Form 94044

Edit your Anthem Form 94044 form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your Anthem Form 94044 form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing Anthem Form 94044 online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit Anthem Form 94044. Replace text, adding objects, rearranging pages, and more. Then select the Documents tab to combine, divide, lock or unlock the file.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
It's easier to work with documents with pdfFiller than you can have ever thought. Sign up for a free account to view.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out Anthem Form 94044

How to fill out Anthem Form 94044
01
Start by downloading the Anthem Form 94044 from the official website or obtaining a physical copy.
02
Read the instructions carefully before filling out the form.
03
Provide your personal information: Name, Address, Phone Number, and Email.
04
Fill in your insurance details, including policy number and type of coverage.
05
Indicate the reason for your request, if applicable.
06
Review the form for any errors or missing information.
07
Sign and date the form at the bottom to validate your request.
08
Submit the completed form via mail or online as directed.
Who needs Anthem Form 94044?
01
Individuals seeking to enroll in or update their information for Anthem healthcare plans.
02
Members who need to submit claims or requests for benefits under their Anthem insurance policy.
03
Applicants needing assistance with medical coverage eligibility or changes.
Fill
form
: Try Risk Free






People Also Ask about
What does it mean to COBRA insurance?
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
What benefits can be continued under COBRA?
Inpatient and outpatient hospital care, • Physician care, • Surgery and other major medical benefits, • Prescription drugs, and • Dental and vision care. Life insurance and disability benefits are not considered “medical care.” COBRA does not cover plans that provide only life insurance or disability benefits.
What is not a COBRA qualifying event?
Taking a leave of absence under the Family and Medical Leave Act of 1993 (FMLA) is not a COBRA qualifying event because FMLA requires a covered employer to maintain group health plan benefits for an employee so the employee has no coverage loss.
What is the meaning continuation of benefits?
Continuation of Benefits means the Company will pay for the Executive's benefits coverage as applied under the Consolidated Omnibus Budget Reconciliation Act (COBRA) for a period of (12 or 18) months. This will be the full amount charged for COBRA premiums for Health, Dental, Vision & Rx coverage.
How does COBRA work when you leave a job?
COBRA coverage lets you pay to stay on your job-based health insurance for a limited time after your job ends (usually 18 months). You usually pay the full premium yourself, plus a small administrative fee. Contact your employer to learn about your COBRA options.
In which circumstances may the right to elect continued coverage under COBRA?
Under COBRA, participants, covered spouses and dependent children may continue their plan coverage for a limited time when they would otherwise lose coverage due to a particular event, such as divorce (or legal separation).
How long is state continuation in Maryland?
The Maryland mini-COBRA law provides for 18 months of continuation coverage, except in the case of terminations for cause. The employer is required provide an election form within 14 days of request by an employee.
Which of the following is considered a qualifying event under COBRA quizlet?
Which of the following is considered a qualifying event under cobra? Divorce. Other qualifying events include the voluntary termination of employment; an employee's change from full time to part time; or the death of the employee.
What does COBRA coverage include?
Inpatient and outpatient hospital care, • Physician care, • Surgery and other major medical benefits, • Prescription drugs, and • Dental and vision care. Life insurance and disability benefits are not considered “medical care.” COBRA does not cover plans that provide only life insurance or disability benefits.
How long is state continuation in Louisiana?
Qualified beneficiaries may remain on COBRA insurance for up to 18 months. In the case where there is a family event, such as a divorce, legal separation, annulment or a child loses dependent status, those beneficiaries may elect continuation insurance for up to 36 months.
Which of the following events will qualify for COBRA continuation coverage?
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Can I get COBRA if I quit my job?
You have 60 days to enroll in COBRA once your employer-sponsored benefits end. You may even qualify if you quit your job or your hours were reduced. Other COBRA qualifying events include divorce from or death of the covered employee.
What is a COBRA offer letter?
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
When an employee is terminated COBRA provides for the continuation of?
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Is it worth paying for COBRA?
COBRA can save you money on out-of-pocket costs. Employer-sponsored health plans may provide broader networks than non-group health plans if you travel out of state or have more than one home.
What does continuation of coverage mean?
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums. Continuation coverage falls into four categories: COBRA, Cal-COBRA, Conversion, and HIPAA.
How much is a continuation COBRA?
On Average, The Monthly COBRA Insurance Premium Cost Is $400 – 700/month Per Individual.
How long is state continuation in Ohio?
Ohio regulations require continuation coverage for a period of 12 months from the date of loss of coverage. Ohio regulations require notification to the Qualified Beneficiary of their continuation rights no later than 31 days after the date of the loss the of coverage.
Why did I get a letter from COBRA insurance?
The employer who provides group health insurance has up to 45 days from the last day of coverage to send you a COBRA election notice to enroll back into the same plan. This enrollment notice may come directly from the employer or a third-party administrator they may use to manage health insurance continuation.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an electronic signature for signing my Anthem Form 94044 in Gmail?
Use pdfFiller's Gmail add-on to upload, type, or draw a signature. Your Anthem Form 94044 and other papers may be signed using pdfFiller. Register for a free account to preserve signed papers and signatures.
How can I edit Anthem Form 94044 on a smartphone?
You may do so effortlessly with pdfFiller's iOS and Android apps, which are available in the Apple Store and Google Play Store, respectively. You may also obtain the program from our website: https://edit-pdf-ios-android.pdffiller.com/. Open the application, sign in, and begin editing Anthem Form 94044 right away.
Can I edit Anthem Form 94044 on an iOS device?
Yes, you can. With the pdfFiller mobile app, you can instantly edit, share, and sign Anthem Form 94044 on your iOS device. Get it at the Apple Store and install it in seconds. The application is free, but you will have to create an account to purchase a subscription or activate a free trial.
What is Anthem Form 94044?
Anthem Form 94044 is a specific form used for reporting healthcare-related information as mandated by Anthem, a health insurance provider.
Who is required to file Anthem Form 94044?
Typically, healthcare providers and organizations that have a contractual agreement with Anthem to provide services or reimbursements are required to file Anthem Form 94044.
How to fill out Anthem Form 94044?
To fill out Anthem Form 94044, one must provide accurate information as requested on the form, ensuring all necessary details related to patient services and claims are included.
What is the purpose of Anthem Form 94044?
The purpose of Anthem Form 94044 is to ensure compliant reporting of healthcare services provided, facilitating accurate processing of claims and reimbursements.
What information must be reported on Anthem Form 94044?
Information that must be reported on Anthem Form 94044 includes patient identification details, service dates, procedure codes, and insurance claim numbers.
Fill out your Anthem Form 94044 online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Anthem Form 94044 is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.