
Get the free Provider Claim Resubmission /Reconsideration Form Mail to: Aetna Better Health of Ne...
Show details
Provider Claim Resubmission /Reconsideration Form Mails to: Aetna Better Health of Nebraska Attention: Claims Resubmission/Reconsideration P.O. Box 63188 Phoenix, AZ 85082 From: (contact) Phone: Corrected
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign provider claim resubmission reconsideration
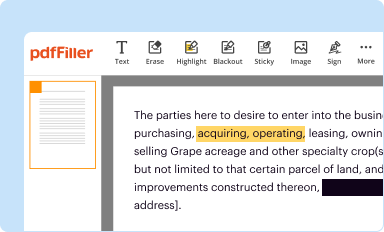
Edit your provider claim resubmission reconsideration form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
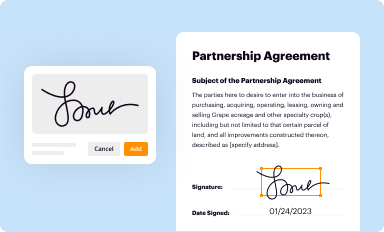
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
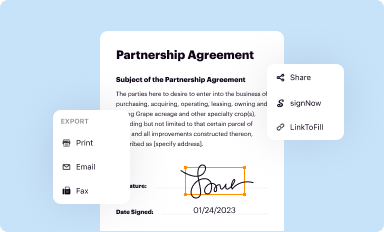
Share your form instantly
Email, fax, or share your provider claim resubmission reconsideration form via URL. You can also download, print, or export forms to your preferred cloud storage service.
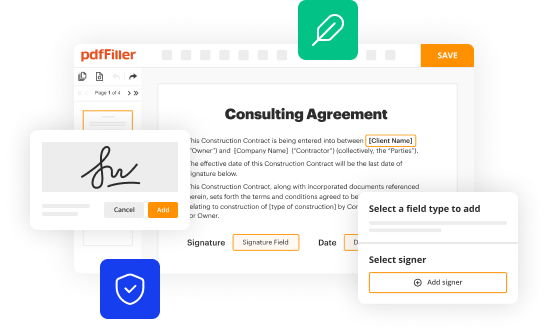
Editing provider claim resubmission reconsideration online
Follow the steps below to benefit from a competent PDF editor:
1
Log in to account. Click on Start Free Trial and sign up a profile if you don't have one.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit provider claim resubmission reconsideration. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
It's easier to work with documents with pdfFiller than you can have ever thought. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out provider claim resubmission reconsideration
How to fill out provider claim resubmission reconsideration:
01
Gather all necessary documentation: Before starting the claim resubmission reconsideration process, make sure you have all the required documents such as the initial claim form, denial letter, and any additional supporting documentation.
02
Review the denial letter: Carefully go through the denial letter to understand why the claim was denied. Note down specific reasons mentioned by the insurance provider as this will help you address those issues in the resubmission.
03
Correct any errors identified: If you notice any errors or discrepancies in the initial claim, it is crucial to correct them before resubmitting. This might involve verifying patient information, service dates, billing codes, or any other relevant details.
04
Provide additional supporting documentation: Along with correcting errors, you may also need to provide additional supporting documentation that was missing in the original claim. This could include medical records, x-rays, lab results, or any other evidence that strengthens your case.
05
Write a detailed explanation: In a separate letter, explain why you believe the claim should be reconsidered. Address each reason mentioned in the denial letter and provide a clear and concise explanation, including any relevant policies or regulations that support your argument. Use a professional and polite tone throughout the letter.
06
Submit the resubmission package: Once you have gathered all the necessary documents and written the letter of explanation, compile them into a resubmission package. Ensure that all documents are organized and clearly labeled. Follow the specific instructions provided by the insurance provider regarding the submission method, such as mailing, faxing, or electronically submitting the package.
Who needs provider claim resubmission reconsideration?
01
Healthcare providers: Doctors, hospitals, clinics, and other healthcare providers who have had their claim denied by an insurance provider may need to go through the claim resubmission reconsideration process.
02
Medical billing and coding professionals: Individuals responsible for preparing and submitting claims on behalf of healthcare providers need to understand the process of provider claim resubmission reconsideration to rectify any denial issues.
03
Patients: Although patients do not directly fill out the provider claim resubmission reconsideration forms, they can play a role in providing essential information or supporting documentation when needed. Understanding the process can help patients advocate for their rights and ensure their claims are reconsidered appropriately.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete provider claim resubmission reconsideration online?
With pdfFiller, you may easily complete and sign provider claim resubmission reconsideration online. It lets you modify original PDF material, highlight, blackout, erase, and write text anywhere on a page, legally eSign your document, and do a lot more. Create a free account to handle professional papers online.
How do I make edits in provider claim resubmission reconsideration without leaving Chrome?
Get and add pdfFiller Google Chrome Extension to your browser to edit, fill out and eSign your provider claim resubmission reconsideration, which you can open in the editor directly from a Google search page in just one click. Execute your fillable documents from any internet-connected device without leaving Chrome.
Can I edit provider claim resubmission reconsideration on an iOS device?
Create, edit, and share provider claim resubmission reconsideration from your iOS smartphone with the pdfFiller mobile app. Installing it from the Apple Store takes only a few seconds. You may take advantage of a free trial and select a subscription that meets your needs.
What is provider claim resubmission reconsideration?
Provider claim resubmission reconsideration is the process of correcting and resubmitting a claim that was previously denied or rejected by an insurance company.
Who is required to file provider claim resubmission reconsideration?
Healthcare providers or their billing staff are typically required to file provider claim resubmission reconsideration.
How to fill out provider claim resubmission reconsideration?
Provider claim resubmission reconsideration should be filled out with the necessary information requested by the insurance company, including details about the original claim and the reasons for resubmission.
What is the purpose of provider claim resubmission reconsideration?
The purpose of provider claim resubmission reconsideration is to correct errors or discrepancies in a claim in order to receive payment for services rendered.
What information must be reported on provider claim resubmission reconsideration?
Provider claim resubmission reconsideration typically requires information such as the patient's name, date of service, diagnosis code, procedure code, and reason for resubmission.
Fill out your provider claim resubmission reconsideration online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Provider Claim Resubmission Reconsideration is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















