Get the free Provider Appeal and Reconsideration Form
Show details
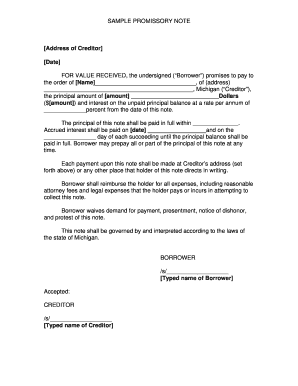
Provider Appeal and Reconsideration Form MONA Dental Louisiana EPS DT and Adult Denture ProgramsThis form is not to be used for initial claim submission or claims adjustments (such as corrected claims).
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign provider appeal and reconsideration
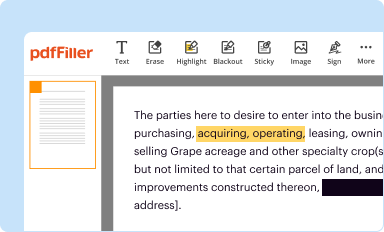
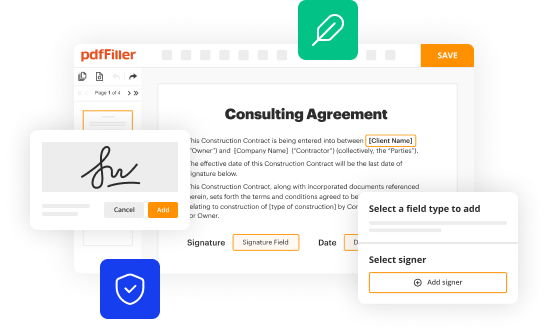
Edit your provider appeal and reconsideration form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
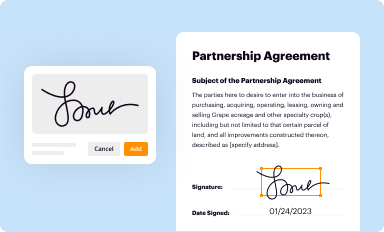
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
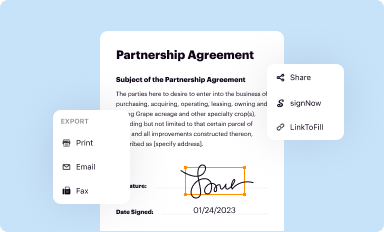
Share your form instantly
Email, fax, or share your provider appeal and reconsideration form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit provider appeal and reconsideration online
Use the instructions below to start using our professional PDF editor:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit provider appeal and reconsideration. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
With pdfFiller, dealing with documents is always straightforward. Try it right now!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out provider appeal and reconsideration
How to fill out provider appeal and reconsideration
01
Step 1: Start by gathering all necessary documentation related to the appeal or reconsideration.
02
Step 2: Review the denial or rejection letter to understand the reason for denial.
03
Step 3: Identify the specific issues that need to be addressed in the appeal or reconsideration.
04
Step 4: Write a clear and concise letter explaining the reasons why the denial or rejection should be overturned.
05
Step 5: Provide supporting evidence or documentation to strengthen your case.
06
Step 6: Submit the appeal or reconsideration letter and supporting documents to the appropriate authority or department.
07
Step 7: Follow up with the authority to ensure that your appeal or reconsideration is being processed and reviewed.
08
Step 8: If necessary, escalate the appeal or reconsideration process by seeking legal assistance or contacting higher authorities.
09
Step 9: Keep track of all correspondence and maintain records for future reference.
10
Step 10: Stay persistent and be prepared for multiple rounds of appeals or reconsideration if needed.
Who needs provider appeal and reconsideration?
01
Anyone who wishes to challenge the denial or rejection of a provider claim can benefit from filing a provider appeal or reconsideration.
02
Healthcare providers, such as doctors, hospitals, clinics, and other medical professionals, may need to file an appeal or reconsideration if their claims are denied by insurance companies or other reimbursement entities.
03
Patients may also indirectly benefit from provider appeal and reconsideration as it can help ensure that their healthcare providers receive the appropriate reimbursement and continue to provide quality care.
04
Billing and coding professionals who handle insurance claims and reimbursement processes may also be involved in filing provider appeals or reconsiderations.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete provider appeal and reconsideration online?
pdfFiller has made it simple to fill out and eSign provider appeal and reconsideration. The application has capabilities that allow you to modify and rearrange PDF content, add fillable fields, and eSign the document. Begin a free trial to discover all of the features of pdfFiller, the best document editing solution.
How do I fill out provider appeal and reconsideration using my mobile device?
You can easily create and fill out legal forms with the help of the pdfFiller mobile app. Complete and sign provider appeal and reconsideration and other documents on your mobile device using the application. Visit pdfFiller’s webpage to learn more about the functionalities of the PDF editor.
How do I edit provider appeal and reconsideration on an iOS device?
You can. Using the pdfFiller iOS app, you can edit, distribute, and sign provider appeal and reconsideration. Install it in seconds at the Apple Store. The app is free, but you must register to buy a subscription or start a free trial.
What is provider appeal and reconsideration?
Provider appeal and reconsideration is the process through which a healthcare provider can challenge a decision made by a health insurance company regarding payment or coverage of services.
Who is required to file provider appeal and reconsideration?
Healthcare providers who disagree with a decision made by a health insurance company are required to file a provider appeal and reconsideration.
How to fill out provider appeal and reconsideration?
To fill out a provider appeal and reconsideration, healthcare providers must follow the specific instructions provided by the health insurance company and submit all relevant documentation.
What is the purpose of provider appeal and reconsideration?
The purpose of provider appeal and reconsideration is to give healthcare providers an opportunity to challenge decisions made by health insurance companies and potentially reverse unfavorable outcomes.
What information must be reported on provider appeal and reconsideration?
Providers must report all pertinent information related to the claim in question, including patient information, services provided, dates of service, and reasons for appealing the decision.
Fill out your provider appeal and reconsideration online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Provider Appeal And Reconsideration is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.