
Get the free prior auth for amerigroup form
Show details
05/02/2014 Prior Authorization Form MARYLAND PHYSICIANS CARE (MEDICAID) (Medicaid) This fax machine is located in a secure location as required by HIPAA regulations. Complete/review information, sign
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign prior auth for amerigroup
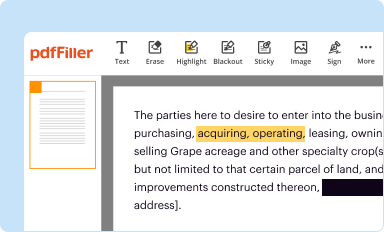
Edit your prior auth for amerigroup form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
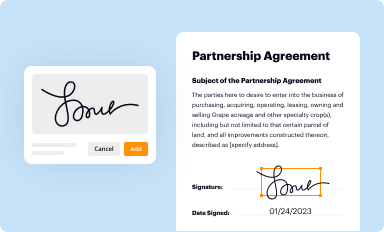
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your prior auth for amerigroup form via URL. You can also download, print, or export forms to your preferred cloud storage service.
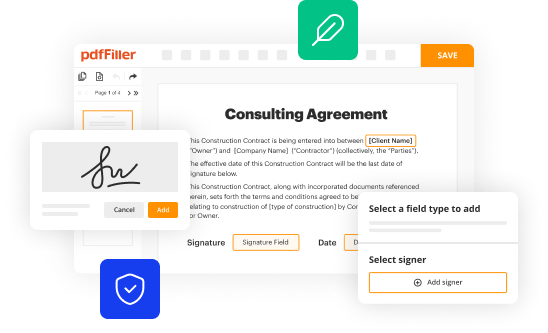
Editing prior auth for amerigroup online
To use our professional PDF editor, follow these steps:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit prior auth for amerigroup. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out prior auth for amerigroup
How to fill out prior auth for Amerigroup?
01
Gather necessary information: Before starting the prior auth process for Amerigroup, make sure to have all the required information at hand. This includes the patient's personal details, insurance information, and the specific medication or treatment for which you are seeking prior authorization.
02
Access the prior auth form: Visit Amerigroup's website or contact their customer service to obtain the prior authorization form. This form is typically available online or can be requested through phone or email.
03
Complete patient information: Fill out the form with the patient's name, date of birth, address, contact information, and insurance details. Double-check the accuracy of the provided information to avoid any processing delays.
04
Provide medical information: Indicate the medical condition or diagnosis that warrants the need for the medication or treatment requiring prior authorization. Include relevant healthcare provider information, such as the name, clinic or hospital, contact details, and their National Provider Identifier (NPI) if available.
05
Include supporting documentation: Attach any necessary supporting documentation, such as medical records, test results, or clinical notes, that provide evidence of the medical necessity for the requested treatment. Ensure that all documents are legible, organized, and clearly referenced on the form.
06
Submit the prior auth form: Once you have completed the form and gathered all the required documents, submit them to Amerigroup using the specified submission method. This can typically be done electronically through their website, by fax, or via mail. Follow any additional instructions provided by Amerigroup for a seamless submission process.
Who needs prior auth for Amerigroup?
01
Patients seeking specific medications: Prior authorization is often required for certain medications that may be expensive, have potential for abuse, or require specific medical justification. Patients who are prescribed such medications may need prior authorization from Amerigroup before their insurance can cover the cost.
02
Individuals requiring specialized treatments or procedures: Some medical treatments or procedures, such as surgeries, imaging studies, or durable medical equipment, may also require prior authorization. This ensures that the requested treatment is medically necessary and meets Amerigroup's coverage criteria.
03
Healthcare providers: Physicians, nurse practitioners, and other healthcare providers who are affiliated with Amerigroup may need to initiate the prior auth process on behalf of their patients. They need to complete the necessary forms and gather the required documentation to support the request for prior authorization.
Remember, the specific requirements and processes for filling out prior auth for Amerigroup may vary, so it is always recommended to refer to the official Amerigroup website or contact their customer service for the most up-to-date and accurate information.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make edits in prior auth for amerigroup without leaving Chrome?
Install the pdfFiller Chrome Extension to modify, fill out, and eSign your prior auth for amerigroup, which you can access right from a Google search page. Fillable documents without leaving Chrome on any internet-connected device.
Can I create an electronic signature for signing my prior auth for amerigroup in Gmail?
You may quickly make your eSignature using pdfFiller and then eSign your prior auth for amerigroup right from your mailbox using pdfFiller's Gmail add-on. Please keep in mind that in order to preserve your signatures and signed papers, you must first create an account.
How can I edit prior auth for amerigroup on a smartphone?
The easiest way to edit documents on a mobile device is using pdfFiller’s mobile-native apps for iOS and Android. You can download those from the Apple Store and Google Play, respectively. You can learn more about the apps here. Install and log in to the application to start editing prior auth for amerigroup.
What is prior auth for amerigroup?
Prior authorization for Amerigroup is a process where healthcare providers need to get approval from the insurance company before providing certain services or medications to their patients.
Who is required to file prior auth for amerigroup?
Healthcare providers such as doctors, hospitals, and pharmacies are required to file prior authorization for Amerigroup.
How to fill out prior auth for amerigroup?
You can fill out prior authorization for Amerigroup by submitting the necessary forms and documentation to the insurance company either online, by fax, or by mail.
What is the purpose of prior auth for amerigroup?
The purpose of prior authorization for Amerigroup is to ensure that the services or medications being requested are medically necessary and appropriate for the patient's condition.
What information must be reported on prior auth for amerigroup?
The information that must be reported on prior authorization for Amerigroup includes the patient's demographic information, the service or medication being requested, supporting medical documentation, and the provider's information.
Fill out your prior auth for amerigroup online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Prior Auth For Amerigroup is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















