Get the free CRITERIA FOR PRIOR AUTHORIZATION - kdheks.gov
Show details
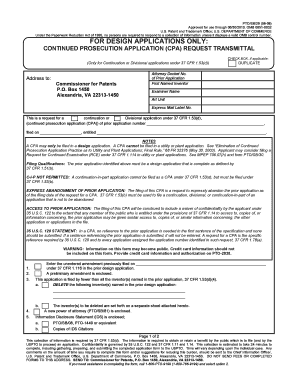
APPROVED PA Criteria Initial Approval: October 10, 2018, CRITERIA FOR PRIOR AUTHORIZATION Calcining Generated Peptide(CORP) Antagonists PROVIDER GROUP:PharmacyMANUAL GUIDELINES: All dosage forms of
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign criteria for prior authorization

Edit your criteria for prior authorization form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your criteria for prior authorization form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing criteria for prior authorization online
Use the instructions below to start using our professional PDF editor:
1
Check your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit criteria for prior authorization. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Save your file. Select it from your list of records. Then, move your cursor to the right toolbar and choose one of the exporting options. You can save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud, among other things.
Dealing with documents is always simple with pdfFiller.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out criteria for prior authorization

How to fill out criteria for prior authorization
01
To fill out criteria for prior authorization, follow these steps:
02
Review the specific criteria requirements outlined by the payer or insurance company.
03
Gather all relevant medical records and documentation supporting the need for the requested healthcare service or treatment.
04
Ensure that the medical records include necessary information such as diagnosis, patient history, and treatment plans.
05
Complete the prior authorization form provided by the payer or insurance company.
06
Provide all required information accurately and thoroughly on the form.
07
Attach the supporting medical records and documentation to the prior authorization form.
08
Submit the completed form and supporting documents to the designated department or contact of the payer or insurance company.
09
Follow up with the payer or insurance company to confirm receipt and track the progress of the prior authorization request.
10
If additional information is requested by the payer or insurance company, promptly provide the required details.
11
Stay informed about the status of the prior authorization request and follow any additional instructions or actions provided by the payer or insurance company.
Who needs criteria for prior authorization?
01
Criteria for prior authorization is often required by healthcare providers, medical professionals, or facilities who need approval from the payer or insurance company before certain healthcare services, treatments, medications, or procedures can be covered or reimbursed.
02
It can also be required for patients who have specific insurance plans or coverage policies that mandate prior authorization for certain healthcare services.
03
Ultimately, anyone seeking healthcare services or treatments that fall under the guidelines of prior authorization criteria may need to comply with this requirement.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I execute criteria for prior authorization online?
Completing and signing criteria for prior authorization online is easy with pdfFiller. It enables you to edit original PDF content, highlight, blackout, erase and type text anywhere on a page, legally eSign your form, and much more. Create your free account and manage professional documents on the web.
How do I fill out criteria for prior authorization using my mobile device?
You can easily create and fill out legal forms with the help of the pdfFiller mobile app. Complete and sign criteria for prior authorization and other documents on your mobile device using the application. Visit pdfFiller’s webpage to learn more about the functionalities of the PDF editor.
How do I complete criteria for prior authorization on an Android device?
Use the pdfFiller Android app to finish your criteria for prior authorization and other documents on your Android phone. The app has all the features you need to manage your documents, like editing content, eSigning, annotating, sharing files, and more. At any time, as long as there is an internet connection.
What is criteria for prior authorization?
Criteria for prior authorization is a set of guidelines or requirements that must be met before certain medical services or treatments will be approved for coverage by insurance companies.
Who is required to file criteria for prior authorization?
Healthcare providers, such as doctors or hospitals, are required to submit criteria for prior authorization to insurance companies before providing certain medical services or treatments.
How to fill out criteria for prior authorization?
Criteria for prior authorization can be filled out by healthcare providers using forms provided by insurance companies, which typically require detailed information about the patient's condition, the proposed treatment, and the medical necessity.
What is the purpose of criteria for prior authorization?
The purpose of criteria for prior authorization is to ensure that medical services or treatments are appropriate, medically necessary, and cost-effective before they are approved for coverage by insurance companies.
What information must be reported on criteria for prior authorization?
Criteria for prior authorization typically require information about the patient's medical history, diagnosis, treatment plan, and any other relevant documentation to support the request for coverage.
Fill out your criteria for prior authorization online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Criteria For Prior Authorization is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.