Get the free Coordination of benefits (COB) is used by benefit carriers to pay health care expens...
Show details
Coordination of Benefits
Coordination of benefits (COB) is used by benefit carriers to pay health care expenses when a patient
is covered by more than one plan. Delta Dental follows legal guidelines
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign coordination of benefits cob
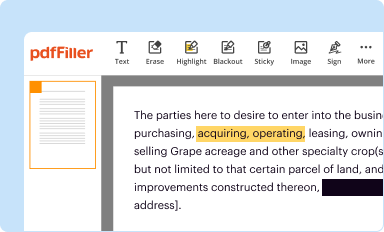
Edit your coordination of benefits cob form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
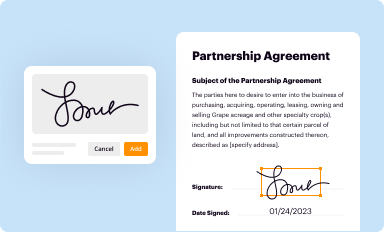
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
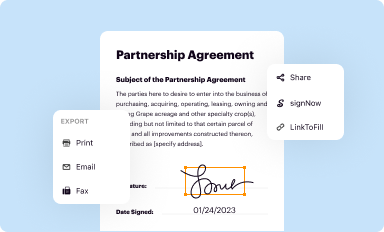
Share your form instantly
Email, fax, or share your coordination of benefits cob form via URL. You can also download, print, or export forms to your preferred cloud storage service.
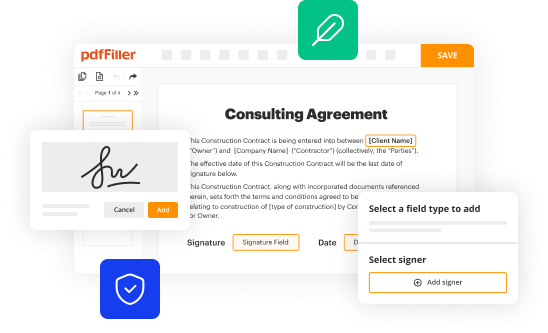
Editing coordination of benefits cob online
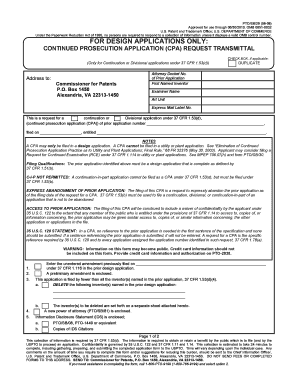
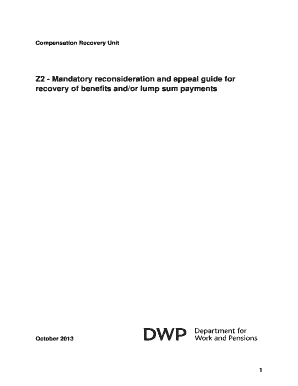
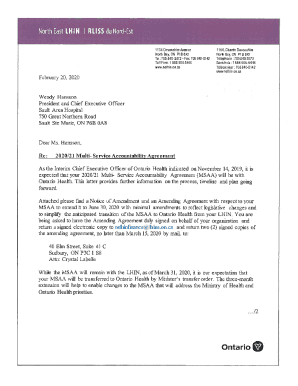
Follow the steps below to take advantage of the professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit coordination of benefits cob. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out coordination of benefits cob
How to fill out coordination of benefits cob
01
Gather necessary information: Collect all relevant health insurance information, including policy numbers, provider contact information, and any applicable claim forms.
02
Identify primary and secondary coverage: Determine which insurance plan is the primary payer and which is the secondary payer. The primary plan typically pays claims first, while the secondary plan covers some or all remaining expenses.
03
Notify both insurance providers: Contact the primary insurance provider to inform them of any secondary coverage. Also, notify the secondary insurance provider about the primary coverage.
04
Submit claims to the primary insurer: File any claims with the primary insurance provider according to their guidelines and procedures. Include all necessary documentation, such as itemized bills and Explanation of Benefits (EOB) statements.
05
Obtain Explanation of Benefits (EOB) statements: Once the primary insurer has processed the claims, you will receive EOB statements outlining the coverage and payments. Keep these for reference when submitting claims to the secondary insurer.
06
Submit claims to the secondary insurer: After receiving the EOB statements from the primary insurer, submit the remaining balance or unpaid claims to the secondary insurance provider. Follow their claims submission process and provide all required documentation.
07
Coordinate payment between insurers: The secondary insurance provider will review the claims and EOB statements to determine their coverage responsibility. They will make the necessary payments to cover the remaining balance, if applicable.
08
Track claim status and payments: Keep track of the claim status and payments from both insurance providers. Follow up if there are any delays or issues in processing the claims.
09
Understand coordination of benefits rules: Familiarize yourself with the coordination of benefits rules and guidelines set by your insurance providers. This will help you navigate the process more effectively.
10
Review and appeal any claim denials: If any claims are denied by either insurance provider, review the reasons for denial and follow the necessary appeals process to resolve the issue.
Who needs coordination of benefits cob?
01
Coordination of Benefits (COB) is needed by individuals who have multiple health insurance plans. This usually occurs when a person is covered by their own insurance as well as a policy provided by their spouse, employer, or government program. COB ensures that the total benefits paid by the multiple plans do not exceed the actual expenses incurred by the individual.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send coordination of benefits cob to be eSigned by others?
To distribute your coordination of benefits cob, simply send it to others and receive the eSigned document back instantly. Post or email a PDF that you've notarized online. Doing so requires never leaving your account.
How do I complete coordination of benefits cob online?
Easy online coordination of benefits cob completion using pdfFiller. Also, it allows you to legally eSign your form and change original PDF material. Create a free account and manage documents online.
How do I edit coordination of benefits cob in Chrome?
Add pdfFiller Google Chrome Extension to your web browser to start editing coordination of benefits cob and other documents directly from a Google search page. The service allows you to make changes in your documents when viewing them in Chrome. Create fillable documents and edit existing PDFs from any internet-connected device with pdfFiller.
What is coordination of benefits cob?
Coordination of Benefits (COB) is a process used in the insurance industry to determine which health insurance plan will pay first when an individual is covered by more than one plan.
Who is required to file coordination of benefits cob?
The insurance companies or healthcare providers are required to file coordination of benefits (COB) when a patient has multiple insurance coverage.
How to fill out coordination of benefits cob?
To fill out coordination of benefits (COB), the insurance company or healthcare provider must collect all relevant insurance information from the patient and submit the claim to the primary insurance first, then the secondary insurance.
What is the purpose of coordination of benefits cob?
The purpose of coordination of benefits (COB) is to ensure that the total amount paid by all insurance plans does not exceed the total cost of the claim, preventing overpayment and decreasing healthcare costs overall.
What information must be reported on coordination of benefits cob?
The information that must be reported on coordination of benefits (COB) includes the name and policy number of each insurance plan, the relationship between the patient and the policyholder, and any other relevant details about the insurance coverage.
Fill out your coordination of benefits cob online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Coordination Of Benefits Cob is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.