Get the free . prior authorization criteria - Fallon Health
Show details
Prescriber Fax Formally Total Care (abiraterone) (Coverage Determination) This fax machine is located in a secure location as required by HIPAA regulations. Complete/review information, sign and date.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign prior authorization criteria
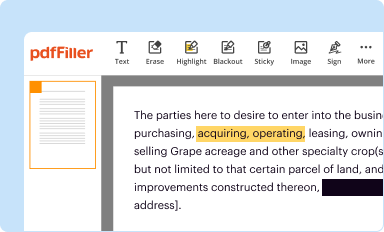
Edit your prior authorization criteria form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
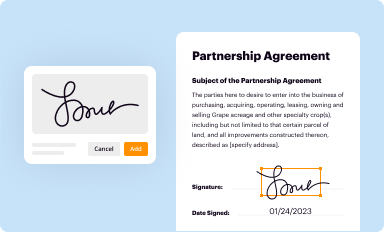
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
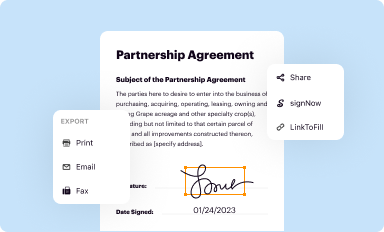
Share your form instantly
Email, fax, or share your prior authorization criteria form via URL. You can also download, print, or export forms to your preferred cloud storage service.
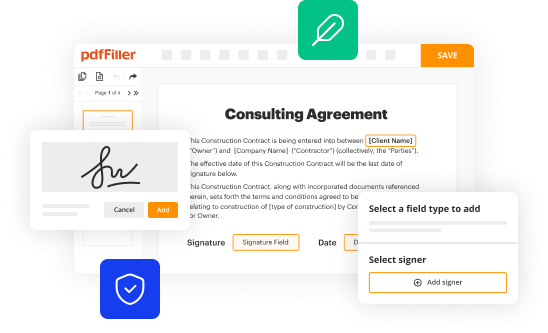
Editing prior authorization criteria online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Log into your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit prior authorization criteria. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
It's easier to work with documents with pdfFiller than you can have ever thought. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out prior authorization criteria
How to fill out prior authorization criteria
01
To fill out prior authorization criteria, follow these steps:
02
Gather all relevant medical records and documentation to support the request for prior authorization.
03
Review the specific criteria outlined by the insurance provider or healthcare organization. This may include clinical guidelines, treatment algorithms, or specific documentation requirements.
04
Ensure that the requested treatment or service meets the defined criteria for prior authorization.
05
Complete the required prior authorization form or document provided by the insurance provider or healthcare organization. Provide accurate and detailed information about the patient, requested treatment or service, diagnosis, and supporting documentation.
06
Submit the completed prior authorization form along with all supporting documents via the designated method specified by the insurance provider or healthcare organization. This can typically be done electronically or through fax.
07
Keep a copy of the submitted prior authorization form and supporting documentation for your records.
08
Monitor the status of the prior authorization request. Follow up with the insurance provider or healthcare organization if there are any delays or if additional information is requested.
09
Once the prior authorization request is approved, proceed with scheduling the approved treatment or service for the patient.
10
If the prior authorization request is denied, review the reasons for denial and consider appealing the decision if appropriate.
11
Document all communication, decisions, and outcomes related to the prior authorization process for future reference.
Who needs prior authorization criteria?
01
Prior authorization criteria is typically required by insurance providers and healthcare organizations.
02
Healthcare providers, including physicians, hospitals, and other healthcare professionals, may need to submit prior authorization criteria for specific treatments, procedures, medications, or services.
03
Patients also need to be aware of prior authorization requirements for certain healthcare services and medications, as they may need to work with their healthcare provider to ensure the necessary criteria are met.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify prior authorization criteria without leaving Google Drive?
It is possible to significantly enhance your document management and form preparation by combining pdfFiller with Google Docs. This will allow you to generate papers, amend them, and sign them straight from your Google Drive. Use the add-on to convert your prior authorization criteria into a dynamic fillable form that can be managed and signed using any internet-connected device.
Where do I find prior authorization criteria?
It's simple with pdfFiller, a full online document management tool. Access our huge online form collection (over 25M fillable forms are accessible) and find the prior authorization criteria in seconds. Open it immediately and begin modifying it with powerful editing options.
How can I fill out prior authorization criteria on an iOS device?
Make sure you get and install the pdfFiller iOS app. Next, open the app and log in or set up an account to use all of the solution's editing tools. If you want to open your prior authorization criteria, you can upload it from your device or cloud storage, or you can type the document's URL into the box on the right. After you fill in all of the required fields in the document and eSign it, if that is required, you can save or share it with other people.
What is prior authorization criteria?
Prior authorization criteria refer to the specific requirements set by insurance companies or health plans that must be met before a healthcare provider can obtain reimbursement for certain medical services, procedures, or medications.
Who is required to file prior authorization criteria?
Healthcare providers, including doctors and specialists, are typically required to file prior authorization requests on behalf of their patients to ensure that the requested services are covered by the patients' insurance plans.
How to fill out prior authorization criteria?
To fill out prior authorization criteria, providers must complete a specific form provided by the insurance company, including pertinent details such as patient information, medical necessity, diagnosis codes, and the requested service or procedure.
What is the purpose of prior authorization criteria?
The purpose of prior authorization criteria is to control healthcare costs, ensure appropriate and necessary care, and prevent misuse or overuse of medical services.
What information must be reported on prior authorization criteria?
Information that must be reported typically includes the patient's demographic details, medical history, diagnosis, proposed service or medication, and any relevant clinical information supporting the request.
Fill out your prior authorization criteria online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Prior Authorization Criteria is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.