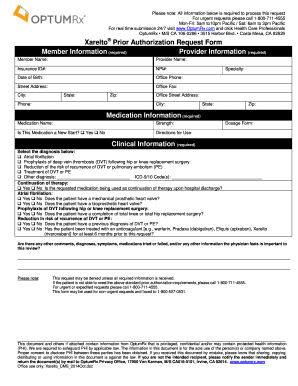
OptumRx Xarelto Prior Authorization Request Form 2017-2026 free printable template
Show details
Opium Rx has partnered with CoverMyMeds to receive prior authorization requests,
saving you time and often delivering reality e determinations.
Visit go.covermymeds.com/OptumRx to begin using this
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign OptumRx Xarelto Prior Authorization Request Form

Edit your OptumRx Xarelto Prior Authorization Request Form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your OptumRx Xarelto Prior Authorization Request Form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit OptumRx Xarelto Prior Authorization Request Form online
To use our professional PDF editor, follow these steps:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit OptumRx Xarelto Prior Authorization Request Form. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. When you find your file in the docs list, click on its name and choose how you want to save it. To get the PDF, you can save it, send an email with it, or move it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Register for an account and see for yourself!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
OptumRx Xarelto Prior Authorization Request Form Form Versions
Version
Form Popularity
Fillable & printabley
How to fill out OptumRx Xarelto Prior Authorization Request Form

How to fill out OptumRx Xarelto Prior Authorization Request Form
01
Obtain the OptumRx Xarelto Prior Authorization Request Form from the official website or your healthcare provider.
02
Complete the patient information section with the patient's full name, date of birth, and insurance details.
03
Fill out the prescriber information including the prescriber's name, contact information, and NPI number.
04
Indicate the patient's diagnosis and provide relevant medical history that supports the need for Xarelto.
05
List any previous medications attempted for the condition and the outcomes.
06
Include the dosage and frequency of Xarelto prescribed by the healthcare provider.
07
Attach any necessary clinical documentation such as lab results or progress notes that justify the use of Xarelto.
08
Sign and date the form, and ensure all sections are completed to avoid delays.
09
Submit the form to OptumRx via the provided fax number or online submission as instructed.
10
Follow up with OptumRx for confirmation and any additional requirements.
Who needs OptumRx Xarelto Prior Authorization Request Form?
01
Patients who have been prescribed Xarelto for a specific medical condition requiring prior authorization.
02
Healthcare providers who are prescribing Xarelto and need to obtain insurance approval for their patients.
03
Insurance companies or pharmacy benefits managers that require verification before covering the cost of Xarelto.
Fill
form
: Try Risk Free






People Also Ask about
How do I get a prior authorization OptumRx?
To begin the PA process, you can: • Let your doctor know that a PA is needed for your medication. Call Optum Rx toll-free at 1-855-828-9834 (TTY: 711). How long does it take for a PA to be approved or denied? Once your PA has been submitted and received, it usually takes 48 to 72 hours to process.
How do I get my doctor to send my prescription to OptumRx?
Your doctor will need to submit a request to OptumRx to confirm that your medication is clinically appropriate for you. Please call (855) 828-9834 (TTY 711) for questions on this process.
How do I appeal a prior authorization denial OptumRx?
Call OptumRx customer service at 888-239-1301 or. Call the OptumRx prior authorization team at 800-711-4555 or. Have your provider fax OptumRx at 844-403-1028.
Why is it so hard to get a prior authorization?
Insurance companies can deny a request for prior authorization for reasons such as: The doctor or pharmacist didn't complete the necessary steps. Filling the wrong paperwork or missing information such as service code or date of birth.
How do I submit a prior authorization to OptumRx?
To begin the PA process, you can: • Let your doctor know that a PA is needed for your medication. Call Optum Rx toll-free at 1-855-828-9834 (TTY: 711). How long does it take for a PA to be approved or denied? Once your PA has been submitted and received, it usually takes 48 to 72 hours to process.
What is the fax number for OptumRx specialty prior authorization?
Fax this form to: 1-866-434-5523 Phone: 1-866-434-5524 OptumRx will provide a response within 24 hours upon receipt.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get OptumRx Xarelto Prior Authorization Request Form?
The pdfFiller premium subscription gives you access to a large library of fillable forms (over 25 million fillable templates) that you can download, fill out, print, and sign. In the library, you'll have no problem discovering state-specific OptumRx Xarelto Prior Authorization Request Form and other forms. Find the template you want and tweak it with powerful editing tools.
How do I make changes in OptumRx Xarelto Prior Authorization Request Form?
With pdfFiller, it's easy to make changes. Open your OptumRx Xarelto Prior Authorization Request Form in the editor, which is very easy to use and understand. When you go there, you'll be able to black out and change text, write and erase, add images, draw lines, arrows, and more. You can also add sticky notes and text boxes.
How do I edit OptumRx Xarelto Prior Authorization Request Form in Chrome?
Adding the pdfFiller Google Chrome Extension to your web browser will allow you to start editing OptumRx Xarelto Prior Authorization Request Form and other documents right away when you search for them on a Google page. People who use Chrome can use the service to make changes to their files while they are on the Chrome browser. pdfFiller lets you make fillable documents and make changes to existing PDFs from any internet-connected device.
What is OptumRx Xarelto Prior Authorization Request Form?
The OptumRx Xarelto Prior Authorization Request Form is a document that healthcare providers must complete to obtain approval from OptumRx for a patient to receive Xarelto, a prescription medication used to prevent blood clots.
Who is required to file OptumRx Xarelto Prior Authorization Request Form?
Healthcare providers, such as physicians or specialists who prescribe Xarelto, are required to file the OptumRx Xarelto Prior Authorization Request Form on behalf of their patients.
How to fill out OptumRx Xarelto Prior Authorization Request Form?
To fill out the form, providers need to include patient information, details about the medical condition being treated, relevant previous treatments, and specific clinical information that supports the need for Xarelto.
What is the purpose of OptumRx Xarelto Prior Authorization Request Form?
The purpose of the form is to ensure that Xarelto is being prescribed appropriately and to confirm that the medication is medically necessary for the patient’s treatment before coverage is granted by OptumRx.
What information must be reported on OptumRx Xarelto Prior Authorization Request Form?
The information required includes patient demographics, diagnosis details, previous medication trials, rationale for choosing Xarelto, and any pertinent medical history that justifies the request.
Fill out your OptumRx Xarelto Prior Authorization Request Form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

OptumRx Xarelto Prior Authorization Request Form is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.