
Get the free Provider Claims Appeal Request Form. Provider Claims Appeal Request Form
Show details
7050 Union Park Center Suite 200 Midvale, UT 84047PROVIDER CLAIMS APPEAL REQUEST FORM Molina Healthcare of Utah/Medicaid/CHIPProvider Information: Provider Name: ___ NPI# ___ Contact Person: ___ Phone:
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign provider claims appeal request
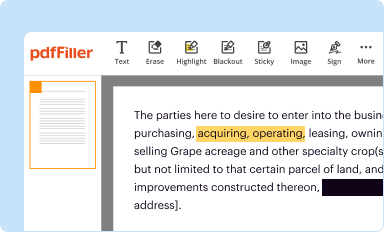
Edit your provider claims appeal request form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
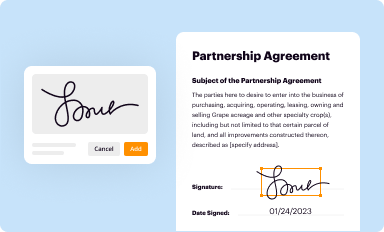
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your provider claims appeal request form via URL. You can also download, print, or export forms to your preferred cloud storage service.
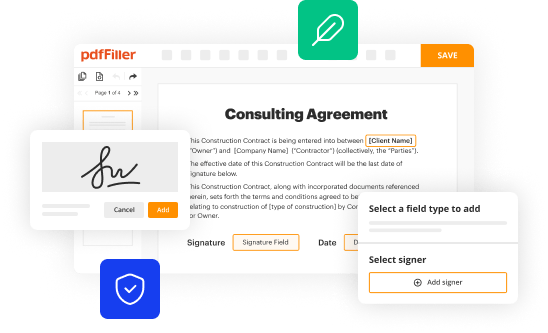
Editing provider claims appeal request online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit provider claims appeal request. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
With pdfFiller, dealing with documents is always straightforward. Try it now!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out provider claims appeal request
How to fill out provider claims appeal request
01
Begin by gathering all the necessary documentation related to the claim you wish to appeal, such as the original claim form, any supporting medical records, and any correspondence with the insurance company.
02
Review the denial letter or explanation of benefits (EOB) provided by the insurance company. Understand the reason for the denial, the specific policy provisions or guidelines that were cited, and what additional information or documentation is required for reconsideration.
03
Prepare a written appeal letter addressing the denial. Clearly state the patient's name, policy or member number, the date of the denial, and reference any claim or denial reference numbers provided by the insurance company.
04
Include a detailed explanation of why you believe the denial is incorrect or unjustified. Provide any additional supporting documentation, such as relevant medical records, test results, or expert opinions.
05
Follow the specific steps outlined by the insurance company for submitting an appeal. This may include filling out a specific appeal request form or submitting the documentation electronically.
06
Keep copies of all documents submitted and consider sending the appeal letter and documentation via certified mail or with a delivery confirmation to ensure proof of receipt.
07
Track the progress of the appeal by following up with the insurance company regularly. Take note of any deadlines or time frames provided for a response.
08
Be prepared to provide any further information or documentation requested by the insurance company during the appeal process.
09
If the appeal is successful, follow up with the insurance company to ensure that the payment is processed and that any necessary adjustments are made to the claim.
10
If the appeal is denied again, review the insurance company's guidelines for further escalation options. This may involve filing a complaint or requesting external review by a third-party organization.
11
Consult with legal or professional advice if necessary, especially if the claim involves a significant amount of money or potential legal implications.
Who needs provider claims appeal request?
01
Provider claims appeal requests are needed by healthcare providers, such as doctors, hospitals, clinics, or other healthcare facilities, who have had a claim denied by an insurance company. These providers need to appeal the denial in order to receive reimbursement for the services or treatments provided to the patient.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete provider claims appeal request online?
pdfFiller has made it easy to fill out and sign provider claims appeal request. You can use the solution to change and move PDF content, add fields that can be filled in, and sign the document electronically. Start a free trial of pdfFiller, the best tool for editing and filling in documents.
How do I edit provider claims appeal request on an iOS device?
Use the pdfFiller mobile app to create, edit, and share provider claims appeal request from your iOS device. Install it from the Apple Store in seconds. You can benefit from a free trial and choose a subscription that suits your needs.
How do I complete provider claims appeal request on an Android device?
Use the pdfFiller Android app to finish your provider claims appeal request and other documents on your Android phone. The app has all the features you need to manage your documents, like editing content, eSigning, annotating, sharing files, and more. At any time, as long as there is an internet connection.
What is provider claims appeal request?
Provider claims appeal request is a formal request submitted by a healthcare provider to challenge a denied claim or request a review of a claim decision.
Who is required to file provider claims appeal request?
Healthcare providers who have had their claims denied or who disagree with a claim decision are required to file a provider claims appeal request.
How to fill out provider claims appeal request?
Providers can fill out a provider claims appeal request by completing the necessary forms provided by the insurance company or third-party payer. They must include relevant information such as patient details, claim number, reasons for appealing, and any supporting documentation.
What is the purpose of provider claims appeal request?
The purpose of a provider claims appeal request is to contest a denied claim or request a reconsideration of a claim decision in order to receive reimbursement for provided services.
What information must be reported on provider claims appeal request?
Provider claims appeal request must include patient details, claim number, reasons for appealing, supporting documentation, and any additional information relevant to the claim.
Fill out your provider claims appeal request online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Provider Claims Appeal Request is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















