
Get the free COBRA HealthPartners Benefits Enrollment/Change Form - shb umn
Show details
Este formulario es para la inscripción opcional de residentes e internos que completan residencias/internados, así como de sus dependientes. Permite la inscripción en COBRA al finalizar la residencia/internado,
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign cobra healthpartners benefits enrollmentchange
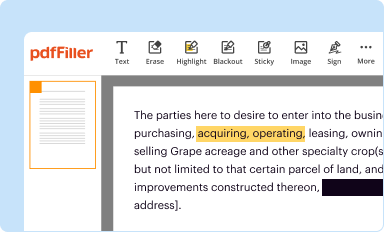
Edit your cobra healthpartners benefits enrollmentchange form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
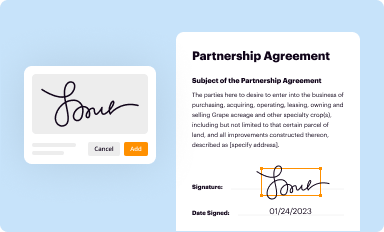
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
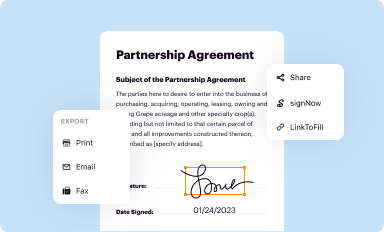
Share your form instantly
Email, fax, or share your cobra healthpartners benefits enrollmentchange form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit cobra healthpartners benefits enrollmentchange online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Log in to account. Start Free Trial and sign up a profile if you don't have one.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
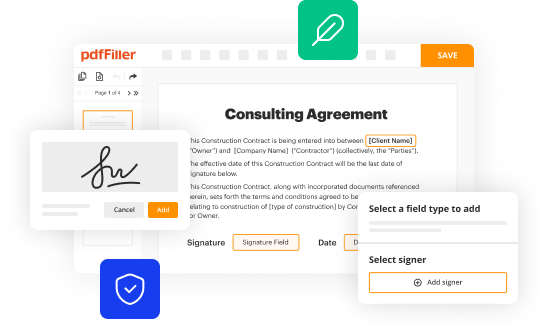
Edit cobra healthpartners benefits enrollmentchange. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
With pdfFiller, dealing with documents is always straightforward. Try it now!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out cobra healthpartners benefits enrollmentchange
How to fill out COBRA HealthPartners Benefits Enrollment/Change Form
01
Obtain the COBRA HealthPartners Benefits Enrollment/Change Form from your employer or the HealthPartners website.
02
Read the instructions provided on the form carefully.
03
Fill in your personal information including your name, address, and contact details.
04
Indicate the reason for enrollment or change in coverage.
05
Provide information about any dependents who will be covered under your plan.
06
Select the health plan option you wish to enroll in or change to.
07
Review the coverage options and costs associated with each selection.
08
Sign and date the form to certify that all information is accurate.
09
Submit the completed form to the designated HR department or COBRA administrator.
Who needs COBRA HealthPartners Benefits Enrollment/Change Form?
01
Employees who have experienced a qualifying event, such as job loss, reduction in hours, or other life events that affect health insurance coverage.
02
Dependents of employees who wish to maintain health coverage after a qualifying event.
Fill
form
: Try Risk Free






People Also Ask about
Is UnitedHealthcare the same as HealthPartners?
A big change is happening between UnitedHealthcare and HealthPartners. It has been noticed that the UnitedHealthcare partnership ends with HealthPartners and they won't work together. The HealthPartners and UnitedHealthcare separation affects 30,000 users and must find new insurers or providers.
What does HealthPartners insurance cover?
Covered services typically include regular office visits with your doctor, tests, urgent and emergency care, hospital stays, prescription drugs, medical equipment and more.
How do I contact HealthPartners customer service?
As a HealthPartners member, you have personal support when you need it. Contact us when you have questions about your coverage or your health – we're here to help. Call the Member Services phone number listed on the back of your Member ID card. Or call 952-883-6677, 888-487-4442 or 952-883-5127 (TTY).
What is a letter of medical necessity for HealthPartners?
By submitting this letter of medical necessity, you certify that the expenses you are claiming are a direct result of the medical condition described, and you would not incur the expenses you are claiming if you were not treating this medical condition.
Did HealthPartners and Park Nicollet merger?
2013. Park Nicollet Health Services and HealthPartners combine. Park Nicollet Health Services includes Methodist Hospital , Struthers Parkinson's Center , Melrose Center and TRIA Orthopedics .
Who did HealthPartners merge with?
In 1992, Group Health merged with MedCenters Health Plan. Together, they formed HealthPartners. Since then, we've combined with notable care organizations. They include Park Nicollet Health System, Regions Hospital, Lakeview Health, and Hudson Hospital & Clinic.
Did HealthPartners change their name?
HealthCare Partners is a division of DaVita Inc., a Fortune 500® company that, through its operating divisions, provides a variety of health care services to patient populations throughout the United States and abroad.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is COBRA HealthPartners Benefits Enrollment/Change Form?
The COBRA HealthPartners Benefits Enrollment/Change Form is a document that allows individuals to enroll in or make changes to their health benefits under the COBRA (Consolidated Omnibus Budget Reconciliation Act) provisions.
Who is required to file COBRA HealthPartners Benefits Enrollment/Change Form?
Individuals who have experienced a qualifying event that affects their health coverage, such as job loss, reduction in hours, or other life changes that impact eligibility, must file the COBRA HealthPartners Benefits Enrollment/Change Form.
How to fill out COBRA HealthPartners Benefits Enrollment/Change Form?
To fill out the COBRA HealthPartners Benefits Enrollment/Change Form, individuals should provide personal information, specify the type of changes or enrollment they are requesting, and submit the form to the appropriate HR or benefits department in a timely manner.
What is the purpose of COBRA HealthPartners Benefits Enrollment/Change Form?
The purpose of the COBRA HealthPartners Benefits Enrollment/Change Form is to facilitate the continuation of health insurance coverage for individuals who would otherwise lose their benefits due to certain qualifying events.
What information must be reported on COBRA HealthPartners Benefits Enrollment/Change Form?
The information that must be reported includes the individual's name, contact details, the qualifying event that triggers COBRA coverage, and any specific changes or requests related to health plan enrollment.
Fill out your cobra healthpartners benefits enrollmentchange online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Cobra Healthpartners Benefits Enrollmentchange is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















