
Get the free Medicare Carriers Manual - Claims Process
Show details
This document outlines the process for filing claims for Medicare payment, detailing definitions, claim requirements, time limits, and procedures for dealing with claims processing, including methods
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign medicare carriers manual
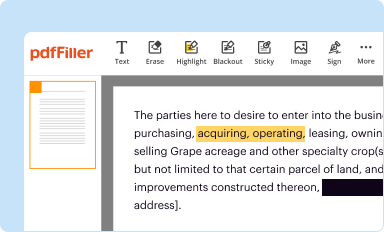
Edit your medicare carriers manual form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
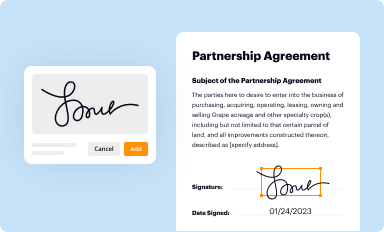
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
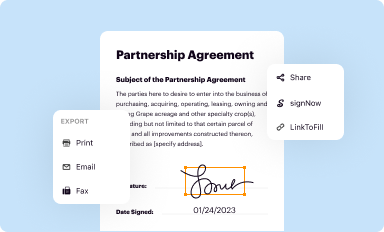
Share your form instantly
Email, fax, or share your medicare carriers manual form via URL. You can also download, print, or export forms to your preferred cloud storage service.
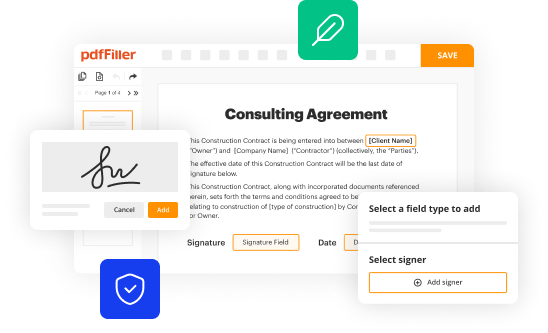
Editing medicare carriers manual online
To use our professional PDF editor, follow these steps:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit medicare carriers manual. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
With pdfFiller, it's always easy to work with documents. Check it out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out medicare carriers manual
How to fill out Medicare Carriers Manual - Claims Process
01
Gather the necessary documentation, including patient information and claim details.
02
Review the specific guidelines outlined in the Medicare Carriers Manual regarding claim submission.
03
Complete the required claim form with accurate information as per the guidelines.
04
Attach supporting documents such as receipts and medical records to validate the claim.
05
Submit the claim electronically or via mail, ensuring that it is sent to the correct carrier.
06
Follow up on the claim status to ensure timely processing and address any issues that arise.
Who needs Medicare Carriers Manual - Claims Process?
01
Healthcare providers submitting claims to Medicare.
02
Billing specialists involved in the claims process.
03
Administrative staff managing patient records and billing.
04
Patients seeking reimbursement for medical services covered by Medicare.
Fill
form
: Try Risk Free






People Also Ask about
What is the first step in submitting a Medicare claim?
Follow these steps: Fill out the claim form provided by your insurance company (if required). Attach copies of the bills you are submitting for payment (if required). Attach copies of the MSN related to those bills. Make copies of everything for your personal records.
What is the Medicare Benefit Policy Manual?
What is the Medicare Benefit Policy Manual? The Medicare Benefit Policy Manual, also known as Publication 100-02, is an online-only reference for Medicare health care providers. This official government document details specific rules and regulations that govern the Medicare program.
Who is the organization that processes Medicare claims for CMS?
The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
Who do Medicare administrative contractors process Medicare claims for?
What's a MAC and what do they do? A Medicare Administrative Contractor (MAC) is a private health care insurer that has been awarded a geographic jurisdiction to process Medicare Part A and Part B (A/B) medical claims or Durable Medical Equipment (DME) claims for Medicare Fee-For-Service (FFS) beneficiaries.
Who is the organization that processes Medicare claims for CMS?
The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
What is the role of the Medicare independent contractor in the claims process?
Qualified Independent Contractors (QICs) The QICs are responsible for conducting the second level of appeals of Medicare claims. The MAC is responsible for handling the first level of appeals. There are 5 QIC jurisdictions: Part A East, Part A West, Part B North, Part B South, and one DME Jurisdiction QIC.
Do Medicare administrative contractors review claims?
[Tara Bernabe] Sure. Medicare Administrative Contractors, also called MACs, play a critical role in the Medicare program. Their responsibilities include things like processing claims, collecting overpayments, enrolling health care providers, and handling appeals.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Medicare Carriers Manual - Claims Process?
The Medicare Carriers Manual - Claims Process is a comprehensive guide that outlines how to submit claims for medical services and procedures covered by Medicare. It provides instructions for providers on the proper codes, documentation, and submission processes necessary for reimbursement.
Who is required to file Medicare Carriers Manual - Claims Process?
Healthcare providers and suppliers who provide services covered by Medicare are required to file claims according to the guidelines set forth in the Medicare Carriers Manual - Claims Process. This includes hospitals, physician offices, and other medical facilities.
How to fill out Medicare Carriers Manual - Claims Process?
To fill out the Medicare Carriers Manual - Claims Process, providers must complete a claim form, typically the CMS-1500 or UB-04, including patient information, service details, procedure codes, and the provider's information. It's crucial to follow the specific guidelines within the manual regarding correct coding and documentation.
What is the purpose of Medicare Carriers Manual - Claims Process?
The purpose of the Medicare Carriers Manual - Claims Process is to provide clear and standardized procedures for submitting claims to Medicare, ensuring that providers receive timely and accurate reimbursement for services rendered to Medicare beneficiaries.
What information must be reported on Medicare Carriers Manual - Claims Process?
Information that must be reported includes patient demographics, insurance information, specific service dates, procedure codes, diagnosis codes, and any relevant modifiers or documentation that supports the services billed, as outlined in the manual.
Fill out your medicare carriers manual online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Medicare Carriers Manual is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















